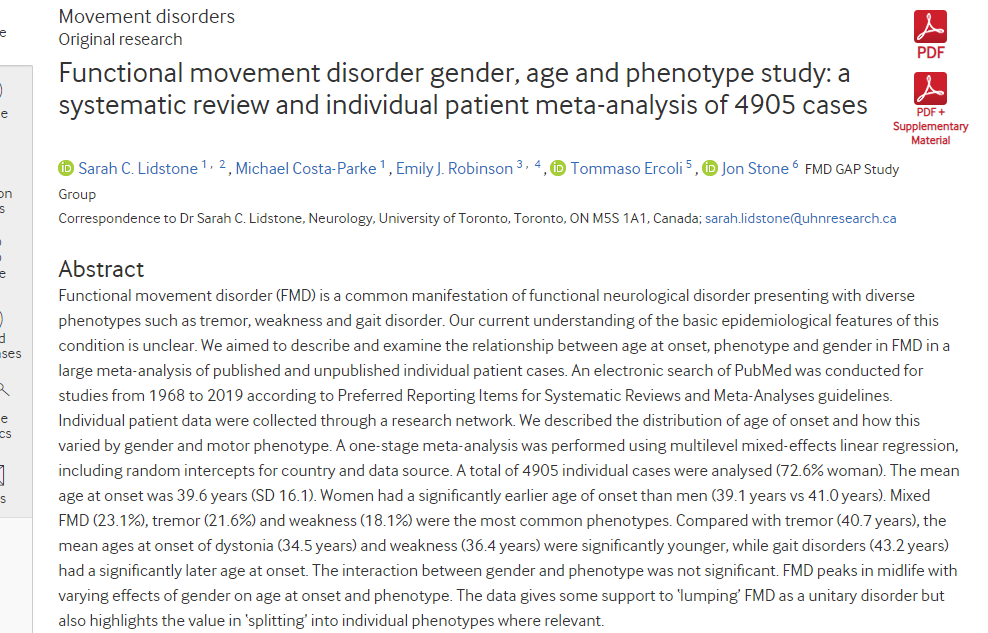
JNNP:功能性运动障碍性别、年龄和表型研究,基于4905例患者的系统回顾和个体荟萃分析
2022-03-03 MedSci原创 MedSci原创
功能性运动障碍(FMD)是功能性神经障碍(FND)的常见临床形式,具有各种运动改变症状,包括震颤、痉挛、肌张力障碍和步态障碍,通常表现为多种表型的组合。
功能性运动障碍(FMD)是功能性神经障碍(FND)的常见临床形式,具有各种运动改变症状,包括震颤、痉挛、肌张力障碍和步态障碍,通常表现为多种表型的组合。尽管存在异质性,但不同形式的FMD患者有着共同的病因风险因素,经历了疼痛或疲劳等重叠症状,并在体检中表现出相同的临床症状,包括可变性和注意力分散。FMD更常见于女性。
尽管FMD流行,但其基本流行病学尚不清楚。大规模流行病学数据由于呈现异质性而受到限制,因为大多数研究都是描述特定表型的较小病例系列。尚不清楚不同的FMD表型是否与发病年龄的差异有关(例如,功能性帕金森病是否在老年人中更常见),或者某些表型是否表现出性别差异。有证据表明,性别比例可能因年龄而异在其他形式的FND发病时。一个由698名功能性癫痫患者组成的大型病例组报告,女性患者的平均发病年龄明显低于男性。本研究收集了大量关于FMD的数据,这些数据来自(1)使用已发表数据进行的系统综述和个体患者数据荟萃分析,以及(2)来自个体研究人员的未发表数据。添加未发表的数据可以可靠地扩充已发表研究之外的数据集。我还计划对功能性癫痫患者的一大组类似数据进行比较。本文发表在《神经病学,神经外科学和精神病学杂志》上().
已发表数据的纳入标准适用于研究层面。如果研究包含满足三个最低标准的个体患者数据,则认为这些研究是合格的:(1)FMD诊断分为“临床确定”或“可能”10.11(2)FMD发病年龄;(3)报告了性别/性别。只包括用英语写的报告。由于大多数数据集依赖于患者/临床医生对确定性别的自我报告,我们选择使用这个术语。因此,我们在本报告中使用了“女性”和“男性”这两个术语.未公布数据的纳入标准用于确保个人数据尽可能与公布的数据集一致,并包括:(1)以FMD为主要诊断的患者,包括任何多动或少动运动障碍和肢体无力;(2) 成人和儿童;(3) 由经过运动障碍训练的神经科医生诊断,来自神经科环境。排除标准为:(1)其他FND类型(如功能性发作和感觉症状);(2) 合并其他运动障碍(如帕金森病)的患者;(3) 同时患有FMD和功能性癫痫的患者;(4) 阵发性FMD(发作性FMD和功能性癫痫发作重叠的风险)。根据最常见的FMD表现,FMD表型分为以下10类:震颤、肌张力障碍、步态障碍、虚弱、痉挛/肌阵挛、混合性、面部症状、帕金森病、其他未知/未记录。”“混合型”被列为发病时出现多种表型(如震颤和步态障碍)的病例。
研究流程
数据是从1968年至2019年的高级PubMed搜索中收集的,使用以下关键词:“功能性”、“心理性”或“转换性”;结合以下任何一种情况:“运动”、“运动”、“步态”、“震颤”、“肌张力障碍”、“虚弱”、“肌阵挛”、“抽搐”、“面瘫”、“阵发性”、“痉挛”和“帕金森病”包括“癫痫”、“癫痫”或“癫痫”的标题被排除在外。所有使用与FMD或运动障碍无关的“功能性”一词的标题均被删除。搜索范围扩大,包括所有相关参考文献。此外,其中一名调查人员还使用上述关键词,通过人工搜索确定了其他记录。将文献综述和手工搜索的结果结合起来,删除所有重复项。
总数据集包括4905例通过系统回顾和手工搜索收集的个体FMD病例(n=878)、共享的已发布组级数据(n=570)和共享的未发布数据库(n=3457)。总共有1448例FMD病例来自分析中所有已公布的来源。该队列包括3558名(72.5%)女性患者。平均发病年龄为39.7岁(中位数为39.8岁)。样本中有383例(7.8%)为儿童发病(年龄)≤16) 。样本中10.7%(526例)的发病年龄超过60岁。最常见的表型是混合型FMD(23.0%)和震颤(21.6%),最不常见的是面部症状和帕金森病。共有479人(9.8%)被归类为“其他”或“未知”表型。几乎一半(42%)的数据来自美国,其余病例来自欧洲、澳大利亚、墨西哥和加拿大。非洲、亚洲和南美洲国家。
与临床相关表型女性比例相比,平均发病年龄结果
不同表型的平均发病年龄存在显著差异 。与功能性震颤相比,功能性肌张力障碍的平均发病年龄年轻4.3岁(95%) CI 2.7至6.0 年龄,p<0.001),功能性虚弱较年轻3.7岁(95%) CI 2.1至5.3 年,p<0.001),而功能性步态障碍的发病平均年龄显著变大,为3.2岁(95%可信区间1.4至5.0,p<0.05)。发病年龄与性别和表型之间的差异如图5所示。虽然所有病例都更常见于比例超过70%的女性,但与其他表型相比,帕金森病(51.8%)和急促/肌阵挛(63.7%)在男性中相对更常见,帕金森病也往往发生在年龄稍大的人群中(44.6±12.9%) 年)。面部症状和肌张力障碍在女性中的发生率要高得多(分别为83.6%和78.4%)。然而,当将表型和性别之间的交互作用项纳入多水平混合模型时,这并不显著(p=0.7513)。
与之前的研究相比,这项大型个体患者数据荟萃分析主要以前所未有的分辨率提供了FMD发病年龄、性别及其表型的详细信息。我们承认,发病年龄曲线和性别构成了一个有限的数据集,据此可以得出病理学结论。尽管如此,我们认为这些数据确实为将口蹄疫视为一个单一的实体,以及区分表型具有有效性的实体提供了一些支持。FMD的临床定义是通过常见的病史特征和检查中的阳性体征,包括可变性和注意力分散,但现象学差异在一定程度上有助于将FMD分为不同的疾病。综合不同表型的大量数据集表明,FMD亚型也具有共同的特征(例如,发病时相似的年龄曲线),并具有不同的流行病学特征(例如,功能性肌张力障碍和功能性步态障碍的平均发病年龄之间的10年差异)。这些结果证实了之前规模小得多的研究表明,FMD在女性中更常见(73%–75%),症状最常见于中年。
未来的研究应该纵向跟踪患者,观察随着时间的推移表型的变化,并确定治疗结果与表型和其他生物标志物之间的关联。最后,研究还为卫生服务规划提供了实用性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#荟萃#
143
#功能性运动障碍#
107
#荟萃分析#
83
#功能性#
82
#运动障碍#
92
#表型#
78
#系统回顾#
90