QRB Discovery :MIT开发出新蛋白,或可阻止COVID-19患者出现细胞因子风暴
2020-04-20 佚名 转化医学网
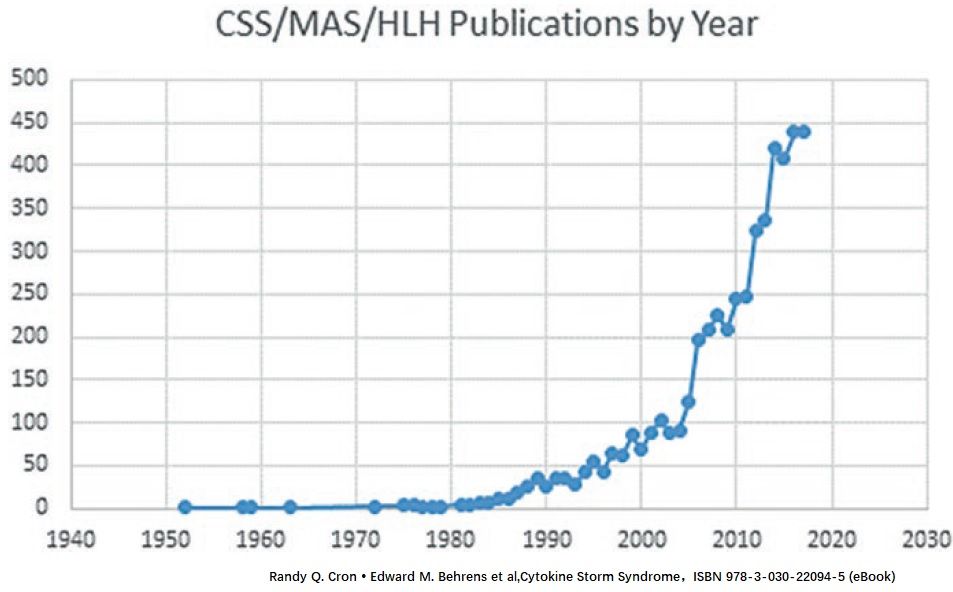
Covid-19的主要特征之一是在严重情况下可能会发生过度的免疫反应。这种免疫过度反应的爆发,也称为细胞因子风暴,会损害肺部并可能致命。细胞因子风暴始终是冠状病毒及其他严重感染患者疾病进展及死亡的重要
Covid-19的主要特征之一是在严重情况下可能会发生过度的免疫反应。这种免疫过度反应的爆发,也称为细胞因子风暴,会损害肺部并可能致命。细胞因子风暴始终是冠状病毒及其他严重感染患者疾病进展及死亡的重要推手之一,所以如何解决免疫过度反应成了科学家的研究关键。
近日,麻省理工学院的研究小组在《生物学评论季刊》(QRB Discovery)杂志上报道了他们的初步发现。他们已经开发出了特殊的蛋白质,其结构类似于抗体,可以吸收过量的细胞因子。体内注射入这种特殊的蛋白质后,它会跟细胞因子风暴产生的过量细胞因子结合,消除过量的细胞因子并减轻感染症状。他们希望开始在人体细胞以及细胞因子释放和冠状病毒感染的动物模型中测试其蛋白质。
好奇心驱动的研究
3月,当证据开始表明SARS-CoV-2病毒正在某些患者体内诱发细胞因子风暴时,研究人员意识到,他们设计的受体蛋白可能会有所帮助。他们决定迅速发布到目前为止所产生的结果,现在他们计划在人细胞和Covid-19感染的动物模型中进行其他测试。
麻省理工学院媒体实验室分子建筑实验室的首席研究科学家张曙光,是该论文的资深作者。他说,这种方法的潜在用途强调了“好奇心驱动的研究”的重要性。事实证明,于2019年4月启动的研究与Covid-19感染患者的治疗直接相关。以好奇心为驱动力,甚至可能是前瞻性的研究通常会促成准备工作,这是预防未来灾难的关键。
分子海绵
张曙光在10年前就开始了这个项目,给了研究人员启发,开展了阻止细胞因子风暴方面的工作,目的是开发修饰型的膜嵌入蛋白。这些蛋白质通常很难研究,因为一旦它们从细胞膜中提取出来,它们只有悬浮在特殊类型的去污剂中才能保持其结构。
经过几年的研究,麻省理工学院的研究科学家Rui Qing和张曙光开发了一种修饰这些蛋白质疏水区域的方法,使它们可溶于水并且易于研究。他们的方法称为数量代码QTY,要求用结构相似的亲水性氨基酸替换一些疏水性氨基酸。亮氨酸转化为谷氨酰胺,异亮氨酸和缬氨酸转化为苏氨酸,苯丙氨酸转化为酪氨酸。
智能生物开发商Avalon GloboCare Corp(AVCO)的首席执行官兼总裁詹建强(David Jin)也是该研究的作者。随着QTY代码的发展,詹建强向张曙光的实验室提出了设计水溶性蛋白(称为细胞因子受体)的想法。这些受体存在于免疫细胞的表面,与细胞因子结合,从而刺激炎症和其他免疫反应。模仿这些细胞因子受体的蛋白质可以帮助抵抗细胞因子风暴,这种风暴可以由病毒或细菌感染(包括HIV和肝炎)产生。它们也可以作为癌症免疫疗法的副作用而发生。
与趋化因子受体类似,QTY码仅适用于这些受体的跨膜结构域,如图1所示。选择红色氨基酸交换以消除设计受体中的疏水斑。细胞外结构域和细胞内连接体都没有受到影响。干扰素和白细胞介素受体的分子量变化很小。
2019年4月,张曙光的团队着手设计可以像海绵一样吸收这些多余细胞因子的蛋白质。为此,他们使用QTY代码制作了细胞因子受体的水溶性版本。当蛋白质溶于水时,它们可以有效地穿越人的血液,而最初的疏水性蛋白质可能会粘附在它们遇到的细胞上。
研究人员还在其水溶性受体蛋白上附加了一个称为Fc区的抗体片段。该区域有助于进一步稳定血液中的蛋白质,并使它们不太可能受到免疫系统的攻击。
研究人员设计了可模仿六种不同细胞因子受体的蛋白质,这些受体可与细胞因子(如干扰素和白介素)结合,并与一类称为趋化因子的细胞因子结合。其中,研究人员选择了两种趋化因子受体的变体(属于7-跨膜(7-TM)G蛋白偶联受体(GPCR)家族),以及4种单跨膜白细胞介素和干扰素受体。相应受体跨膜区的L,I,V,F氨基酸残基被Q,T,Y取代。在对蛋白质结合强度的实验室测试中,研究人员发现它们修饰的蛋白质能够以与天然细胞因子受体相似的强度结合到细胞因子上。他们设计的细胞因子受体将吸收细胞因子风暴期间释放的大多数过量细胞因子。
研究人员还使用基于网络的工具TMHMM Server v2.0分析数量变异蛋白序列,以预测疏水跨膜段的存在。服务器基于一个隐马尔可夫模型(HMM),该模型考虑了跨膜螺旋的实际生物结构,同时计算了存在的可能性。
阻止细胞因子风暴的曙光
在本研究中,QTY编码修饰的变异趋化因子受体CCR9QTY和CXCR2QTY的成功设计进一步扩展了这种蛋白质设计算法在7-TM GPCRs上的可行性。结合之前的工作,实验室在保留其生理和功能特性的同时,成功地设计和工程化了8个可溶性GPCRs变体,包括7个趋化因子受体变体和1个嗅觉受体变体。QTY在地质雷达系统中的普遍适用性,可以进一步促进以功能等效形式对这些先前困难目标的研究。QTY代码可能普遍应用于其他类型的多径膜蛋白和难以表达的蛋白。这些研究正在进行中。虽然体内也存在截短的可溶性白细胞介素和干扰素受体,主要是通过细胞外和跨膜段之间的分裂,但QTY代码对于设计这些单跨膜受体进行进一步研究仍然有意义。
研究人员已为其设计的蛋白质以及创建水溶性细胞因子受体的整体方法申请了专利。他们希望能够快速获得技术许可,并希望与制药和生物技术公司合作,帮助他们将其应用于临床试验。这种方法将需要进一步的动物研究以及潜在的人类临床研究。但这一发现将有助于临床应用来解决涉及细胞因子风暴的病毒性疾病。
参考文献:
Shilei Hao,et al. QTY code-designed water-soluble Fc-fusion cytokine receptors bind to their respective ligands.QRB Discovery (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#cover#
75
#Dis#
89
#胞因子#
71
#MIT#
90
#细胞因子#
85
#COVID-19患者#
76
#ISC#
77