Am Heart J:45岁以上中老年患者中,BNP是肺动脉高压患者死亡率或肺移植的有力预测因素
2022-08-06 MedSci原创 MedSci原创
肺动脉高压(PAH)是一种不常见的疾病,其特点是肺血管重塑,导致肺血管阻力(PVR)增加,造成肺动脉压力增加。在PAH患者的风险分层中,既往研究已经对多种生物标志物进行了调查。
肺动脉高压(PAH)是一种不常见的疾病,其特点是肺血管重塑,导致肺血管阻力(PVR)增加,造成肺动脉压力增加。在PAH患者的风险分层中,既往研究已经对多种生物标志物进行了调查。近日,发表于Am Heart J的一项系统综述和荟萃分析首次研究了(NT-pro)BNP对PAH患者的预后价值。
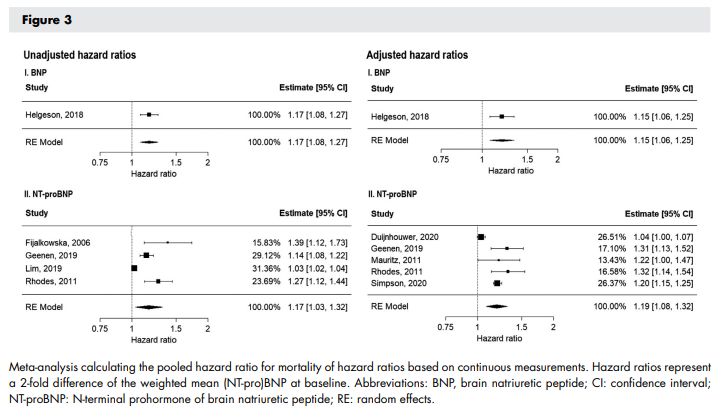
研究人员使用MEDLINE、Embase、Web of Science、Cochrane图书馆和Google scholar进行系统性文献检索,以确定PAH中基线(NT-pro)BNP水平的预后价值的研究。纳入报告死亡率或肺移植终点的危险比(HR)的研究。进行随机效应荟萃分析,计算诊断时(NT-pro)BNP水平的集合HR。为了说明应用于(NT-pro)BNP的不同转换,对于报告基于连续(NT-pro)BNP测量的HR的研究,计算了加权平均(NT-pro)BNP水平247pmol/L的2倍差异的HR。
结果,共纳入16项研究,包括6999名中老年患者(平均年龄45.2-65.0岁,97.3%为PAH)。总的来说,1460名患者在1至10年的平均随访期内达到终点。9项研究报告了基于截止值的HRs。荟萃分析结果显示,NT-proBNP和BNP升高时,死亡或肺移植的风险增加,基于未调整的HRs的集合HRs分别为2.75(95%-CI:1.86-4.07)和3.87(95% CI 2.69-5.57)。六项研究报告了(NT-pro)BNP的继续规模的HR。加权平均NT-proBNP的2倍差异导致死亡或肺移植的风险增加,集合HR为1.17(95%-CI:1.03-1.32)。
综上所述,该研究结果表明,(NT-pro)BNP水平的增加与PAH患者死亡或肺移植的风险明显增加有关。因此,在诊断时,NT-proBNP和BNP是PAH患者死亡率或肺移植的有力预测因素。测量(NT-pro)BNP应该是PAH临床护理和风险分层的基石。
原始出处:
Paul M Hendriks, et al., Prognostic value of brain natriuretic peptides in patients with pulmonary arterial hypertension: A systematic review and meta-analysis. Am Heart J. 2022 Aug;250:34-44. doi: 10.1016/j.ahj.2022.05.006.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#45岁#
58
#肺动脉高压患者#
102
#患者死亡#
68
#中老年#
84
#动脉高压#
71
#预测因素#
0
#BNP#
79
#ART#
95
#HEART#
97