JCO: Ixazomi联合来那度胺+地塞米松治疗复发或难治性多发性骨髓瘤(RRMM)的最终分析结果:III期临床研究TOURMALINE-MM1
2021-06-13 yd2015 MedSci原创
Ixazomib-Rd治疗复发或难治性多发性骨髓瘤(RRMM)的无进展生存(PFS)获益并没有转化为OS的获益。但在某些亚组,Ixazomib-Rd组有OS的获益倾向。
TOURMALINE-MM1研究是一项全球多中心、双盲、安慰剂对照随机III期研究,评估Ixazomib联合来那度胺+地塞米松(Ixazomib-Rd)对比安慰剂联合来那度胺+地塞米松(安慰剂-Rd)在复发或难治性(RR)多发性骨髓瘤(MM)的疗效和安全性。既往已经报道了Ixazomib-Rd 较安慰剂-Rd 明显改善RRMM患者的无进展生存期(PFS)(中位PFS 20.6个月 v 14.7个月; HR=0.74; 95% CI, 0.59 to 0.94;P=0.01)。近期,最终的分析结果发表在Journal of Clinical Oncology杂志上。
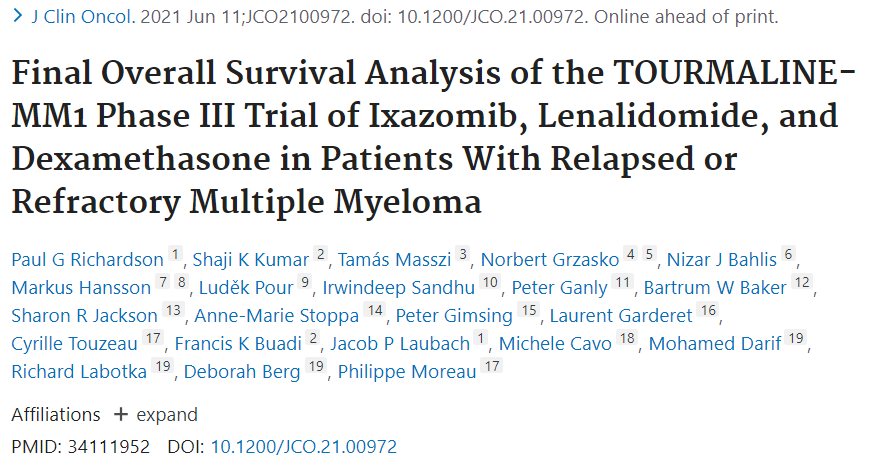
Ixazomib-Rd组有360例患者,而安慰剂-Rd组有362例患者。两组的中位随访时间分别为85.0和85.1个月。两组的中位OS并没有统计学差异,分别为53.6个月(95% CI, 49.25 to62.95)和51.6个月(95% CI,44.78 to 59.14)(HR=0.939; 95% CI, 0.784 to 1.125; P=0.495)。
亚组分析时,发现某些亚组中Ixazomib-Rd有获益的倾向,比如任何线治疗后出现难治(HR=0.794; 95% CI, 0.538 to 1.172);最后线治疗后出现难治(HR=0.742;95%CI, 0.460to 1.198);沙利度胺后难治 (HR=0.781;95% CI, 0.461 to 1.322); > 65-75岁(HR=0.757; 95% CI, 0.559 to 1.027); III期(HR=0.779; 95% CI, 0.487 to 1.247);接受过2-3线治疗(HR=0.845; 95% CI, 0.642 to 1.114); 常规的细胞遗传学风险 (HR=0.875; 95% CI, 0.684to 1.118)。
两组和亚组分析的OS
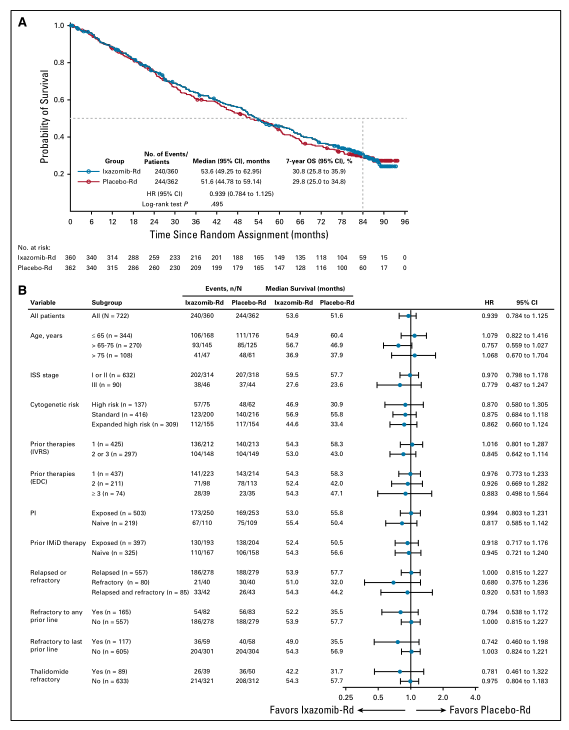
而对下列患者,Ixazomib-Rd治疗取得了OS数值上的获益,伴有del(17p)的患者(HR=0.916; 95% CI, 0.516 to 1.626), 高细胞遗传学风险患者(HR 0.870; 95% CI, 0.580 to 1.305), 扩展的高细胞遗传学风险患者(HR 0.862; 95% CI, 0.660 to 1.124)。高细胞遗传学风险定义为FISH检测的del(17p), t(4;14),和 t(14;16)至少一项阳性。扩展的高细胞遗传学风险定义为del(17p), t(4;14), t(14;16), 和1q21扩增中至少一项阳性。常规的细胞遗传学风险定义为没有高细胞遗传学风险的特征。
不同遗传风险的OS
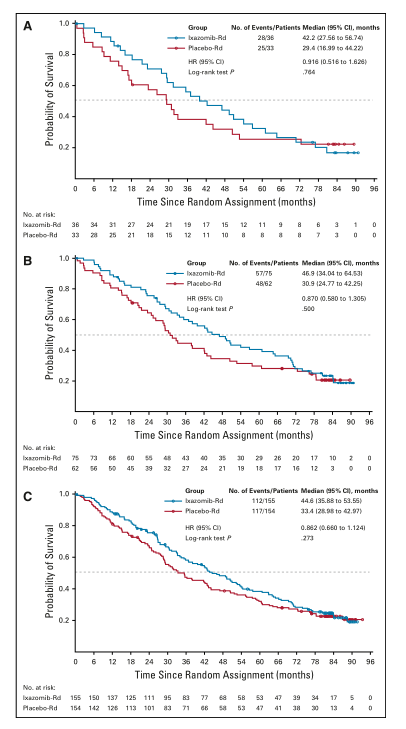
两组中分别有259例患者(71.7%)和251例患者(69.9%)接受≥1的后线治疗,比如daratumuma(24.7% vs 33.9%),bortezomib (56.8% v 61.8%), carfilzomib (27.0% v 33.5%),后线的蛋白酶抑制剂(47.5% v 55.8%)。
两组接受后线蛋白酶抑制剂的中位OS分别为52.0和56.9个月(HR=1.04,95%CI(0.78 to 1.4),p=0.779),不接受后线蛋白酶抑制剂的中位OS分别为54.6和48.8个月(HR=0.9,95%CI( (0.71 to 1.13),p=0.373)。
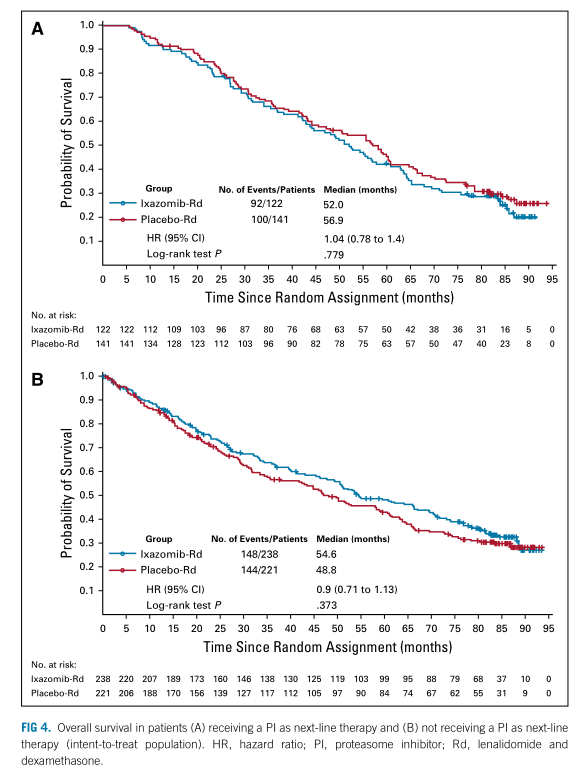
两组接受或不接受后线蛋白酶抑制剂的OS
随访7年时间,没有新的或额外的安全事件发生。两组的不良事件差别超过5%的只有两种,为血小板减少症(21.3% v 10.3%)和腹泻 (10.0% v 3.1%)。两组新的原发恶性肿瘤发生率分别为10.3% 和11.9%。
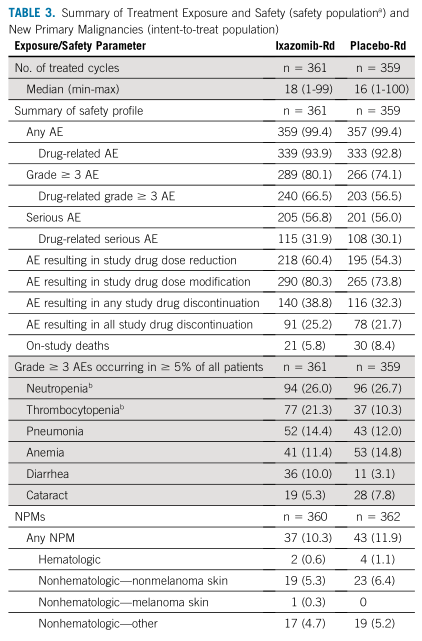
不良事件
综上,Ixazomib-Rd治疗复发或难治性多发性骨髓瘤(RRMM)的无进展生存(PFS)获益并没有转化为OS的获益。但在某些亚组,Ixazomib-Rd组有OS的获益倾向。
原始出处:
Paul G Richardson, Shaji K Kumar, Tamás Masszi, et al. Final Overall Survival Analysis of the TOURMALINE-MM1 Phase III Trial of Ixazomib, Lenalidomide, and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. J Clin Oncol. 2021 Jun 11;JCO2100972. doi: 10.1200/JCO.21.00972. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#I期临床#
87
#III期临床研究#
57
#AZ#
99
#JCO#
58
#多发性#
56
#III#
47
#II期临床研究#
54
#II期临床#
49
#难治性#
64
#III期#
62