Mov Disord : 进行性核上麻痹,言语障碍的灰白质结构基础是什么?
2021-09-23 Freeman MedSci原创
神经解剖学损伤的不同模式与口腔和咽喉阶段的吞咽障碍相对应。
进行性核上性麻痹(PSP)是一种神经退行性tauopathy,以眼球运动功能障碍、姿势不稳和跌倒、运动障碍和认知功能障碍为特征。
 延髓症状往往出现得很早,可以很严重,而且是一个独立的生存预测因素,可能是因为生理性吞咽障碍导致吸入性肺炎的风险增加,这是PSP最常见的死亡原因。
延髓症状往往出现得很早,可以很严重,而且是一个独立的生存预测因素,可能是因为生理性吞咽障碍导致吸入性肺炎的风险增加,这是PSP最常见的死亡原因。
以前关于PSP吞咽困难的报告一直都是以口腔(相对于咽部)的障碍为主。常见的口腔阶段障碍包括来回摇动,或舌头的嵌顿运动,以推动药丸向咽部移动,舌根回缩减少,咽部吞咽的开始时间延迟。
咽相障碍的严重程度和气道侵入的程度与PSP疾病的严重程度有关。初级脑干和核上控制中心支持吞咽,口腔阶段受自愿控制,核上控制中心的影响较大,咽和食道阶段由髓质中央模式发生器驱动。纤维束,包括皮质-球状束和胼胝体,为这个网络的功能服务。然而,对PSP吞咽困难的神经解剖学基础知之甚少。
藉此,美国梅奥诊所的Heather M. Clark等人,探究了灰质体积和白质道的完整性与口腔和咽部的吞咽困难和气道入侵的关系。
并预测口腔阶段的障碍将与 高层皮质吞咽网络有关,而咽部相障碍将与脑干通路。
38名患有进行性核上性麻痹的参与者接受了视频荧光图吞咽评估( videofluorographic swallowing assessment)以及结构和弥散张量头部磁共振成像。线性回归模型评估了吞咽指标与区域灰质体积、白质各向异性和平均扩散率之间的关系。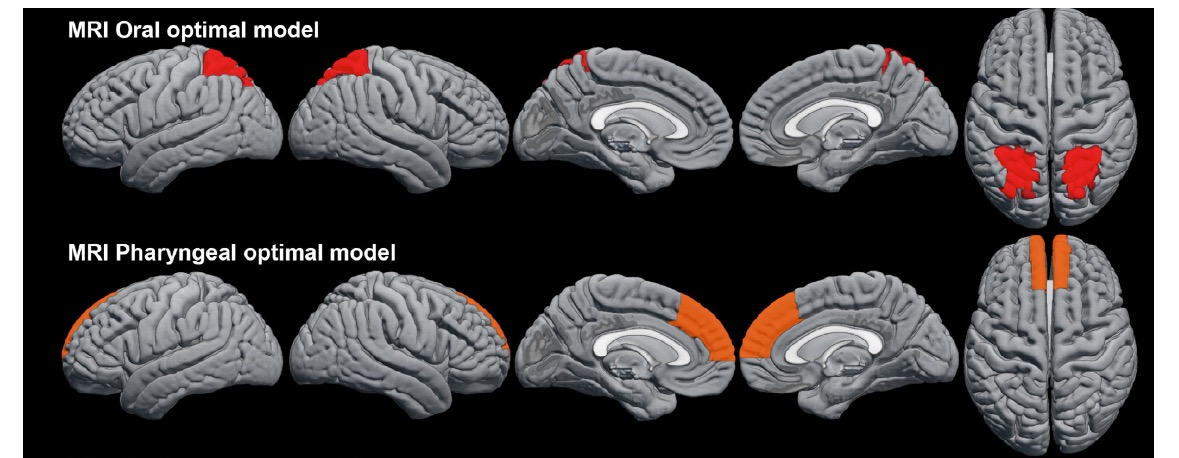
他们发现:口腔阶段的障碍与顶上容积的减少和顶层和感觉运动白质、内囊后肢和上纵筋的异常扩散性有关。咽相损伤与内侧额叶、皮质脊髓束和脑梗的破坏有关。没有任何区域可以预测气道入侵。
这个研究的重要意义在于发现了:神经解剖学损伤的不同模式与口腔和咽喉阶段的吞咽障碍相对应。
原文出处:
Clark HM, Tosakulwong N, Weigand SD, et al. Gray and White Matter Correlates of Dysphagia in Progressive Supranuclear Palsy. Mov Disord. Published online August 23, 2021:mds.28731. doi:10.1002/mds.28731
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Dis#
73
#Disord#
77
#白质#
80
#结构基础#
77
#进行性#
89