OCC 2015 :刘少稳——2014年晕厥诊断与治疗的中国专家共识解读
2015-09-10 MedSci MedSci原创
中华医学会第十七次全国心血管大会暨第九届东方心脏病学会议(OCC2015)今天在上海世博中心隆重举行。今天上午举行的继续教育论坛心律失常场上,来自上海交通大学医学院附属第一人民医院心内科主任刘少稳刚发表题为《2014年晕厥诊断与治疗的中国专家共识解读》主题演讲,精彩内容如下: 指南重点: 从两个方面强调了评价晕厥的患者:一是找出确切的原因以便进行有效的针对病理机制的治疗;二是识别患者的风险
中华医学会第十七次全国心血管大会暨第九届东方心脏病学会议(OCC2015)今天在上海世博中心隆重举行。今天上午举行的继续教育论坛心律失常场上,来自上海交通大学医学院附属第一人民医院心内科主任刘少稳刚发表题为《2014年晕厥诊断与治疗的中国专家共识解读》主题演讲,精彩内容如下:
指南重点:
从两个方面强调了评价晕厥的患者:一是找出确切的原因以便进行有效的针对病理机制的治疗;二是识别患者的风险,这种风险常取决于潜在的疾病而不是晕厥本身的机制。这样是为了避免医生混淆这两个方面。
指南最明显的变化:
流行病学的证据:晕厥是临床上常见的症状,占急诊科患者的0.9%-1.7%,住院患者的1%-3%。
对心脏性猝死(SCD)和心血管事件风险分层的新的诊断策略,包括某些高危不明原因晕厥患者的治疗推荐意见。
强调采取以长时间监测为基础的诊断策略而不是传统以实验室检查为基础的诊断策略。
更新了以循证医学为基础的治疗方法。
指南首明确了晕厥的定义:
晕厥是由于短暂的全脑组织缺血导致的一过性意识丧失(T -LOC);特点为发生迅速、短暂、自限性,并且能够完全回复的意识丧失,但可能造成不同程度的外伤及相应并发症。
癫痫、低血糖、癔病——又称非晕厥性意识丧失。
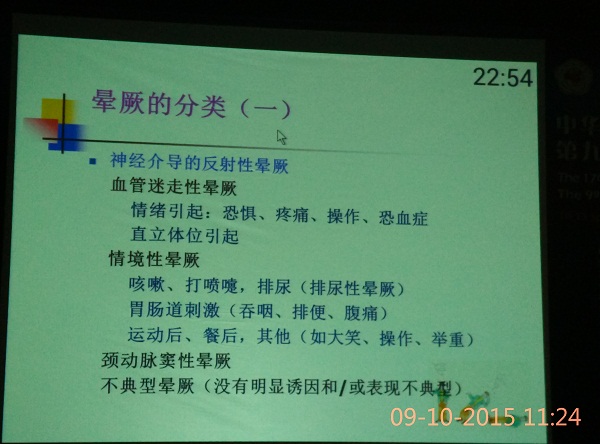
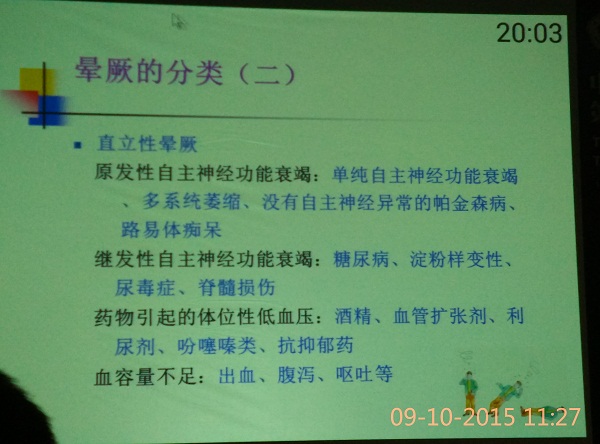
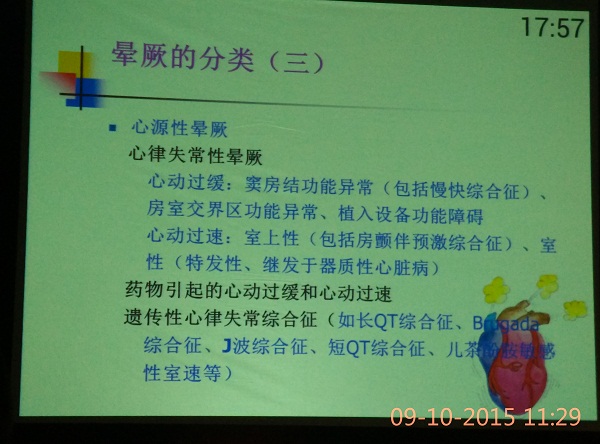
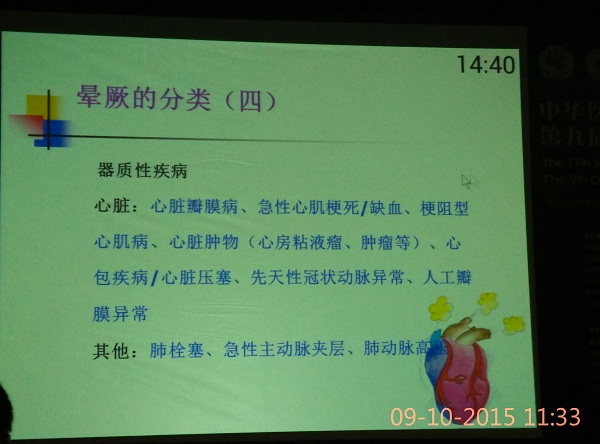
晕厥分类:
指南更新了分类,在短暂意识丧失(T-LOC)的大的框架内对晕厥进行了分类更新。

图:T-LOC分类
纳入了数个新的流行病学资料:
1.迷走性晕厥是导致晕厥最主要原因;心源性晕厥是第二位原因。在小于40岁的患者中,体位性低血压导致的晕厥较少见。
2.个别患者的病情较为复杂,在医疗转诊、救治的过程中,一些非晕厥的意识丧失患者常被误诊为晕厥。
增加了初步评价内容
1.详细询问病史、体格检查(包括测量不同体位血压)以及心电图检查,在此基础上,可以适当增加其他的检查以保证诊断准确。
2.对于有心脏病病史或怀疑此次晕厥与结构性心脏病或其他心血管疾病有关的患者,建议进行超声心动检查;
3.对于怀疑心律失常而导致晕厥的患者,应给予实时心电监测;
4.若晕厥与体位变化有关或怀疑反射性晕厥时,则应进行相关检查。如卧立位试验和/或直立倾斜试验等;
5.仅在怀疑非晕厥原因造成的的一过性意识丧失的情况下,进行神经科检查或血液检查。
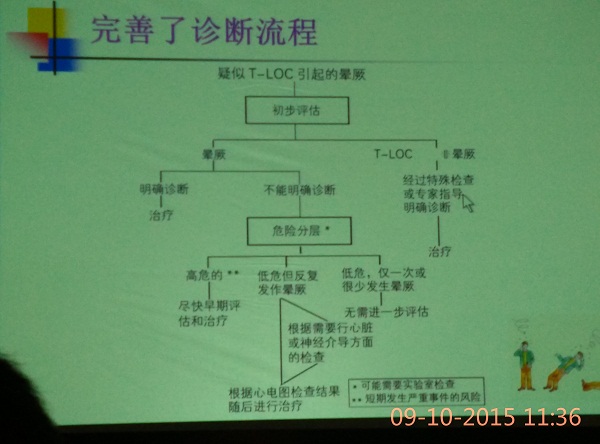
图:完善的诊断流程
检查方法:
颈动脉窦按摩(CSM)
直立激发试验(主动直立和倾斜试验)
ECG、动态心电图或实时心电监测
电生理检查
影像学检查——心脏超声
运动试验
心导管
精神评估
神经评估
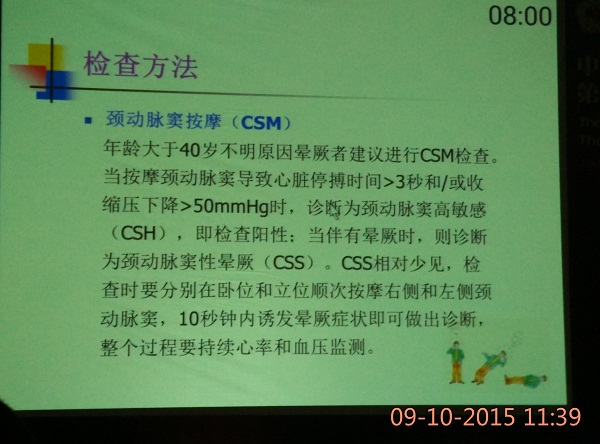
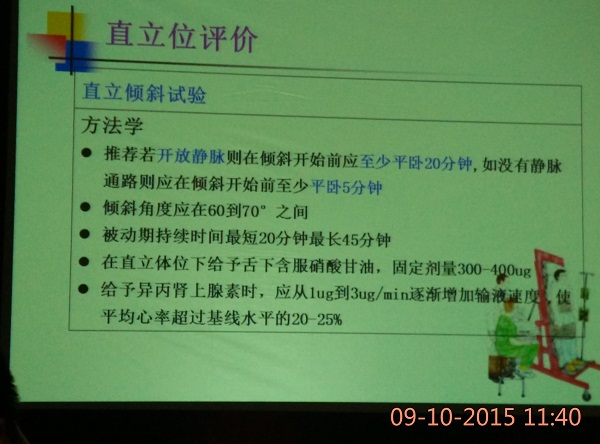
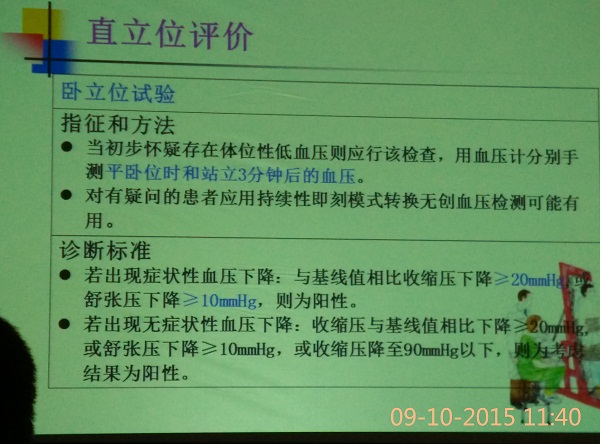

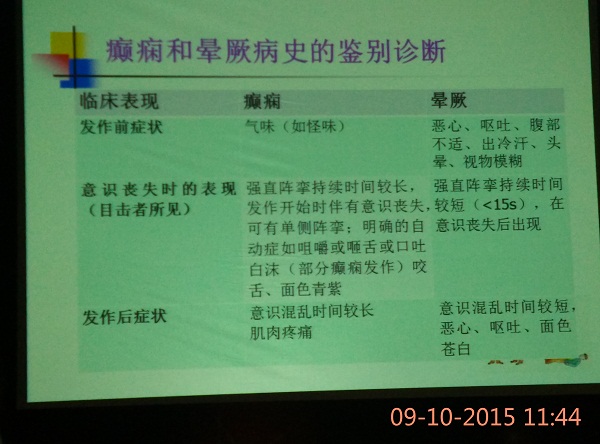
图:癫痫和晕厥病史的鉴别诊断
体位性性低血压和直立性不耐受综合征
1.非药物治疗
1)消除药物作用;2)对无高血压者,应摄入足够的盐和水,每天达到2~3L液体和10g氯化钠;3)起床前锻炼,避免突然改变体位。
更多精彩内容请关注MedSci医学App(点击下载)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#诊断与治疗#
94
#专家共识#
79
#中国专家共识#
71
#晕厥#
94
#OCC#
57
赞
176
赞
182
有见地,是个不错的方向
119
值得学习
129
期待进一步的研究
159