BMJ:多学科讨论(MDT)或会导致过度治疗
2015-09-24 Mechront 译 MedSci原创
对于肿瘤病人临床上通常会进行多学科讨论(MDT)以决定治疗方案。参与MDT的医生包括:肿瘤科、放射科、外科、病理科,以及根据肿瘤组织类型需要的其他相关科室的医生,普遍是年轻医生。Franz Eigenmann在25年前第一次参加MDT,这种讨论方式,对医疗的临时决策提供帮助和保护,并且是有价值的。但是现在变了,许多国家的普遍的感觉似乎是对每一个癌症患者的每一个重大决策上的治疗都应该由MDT来决定。
对于肿瘤病人临床上通常会进行多学科讨论(MDT)以决定治疗方案。参与MDT的医生包括:肿瘤科、放射科、外科、病理科,以及根据肿瘤组织类型需要的其他相关科室的医生,普遍是年轻医生。
Franz Eigenmann在25年前第一次参加MDT,这种讨论方式,对医疗的临时决策提供帮助和保护,并且是有价值的。但是现在变了,许多国家的普遍的感觉似乎是对每一个癌症患者的每一个重大决策上的治疗都应该由MDT来决定。MDT对不确定的诊治是有价值的,但是对于明确适应症的讨论则是浪费资源。还有MDT最后的讨论结果往往是其中最资深的医生所做出的。医疗行为最重要的便是查看患者,这种没有查看病人便做出这至关重要的决策是不可被接受的。
集体决策
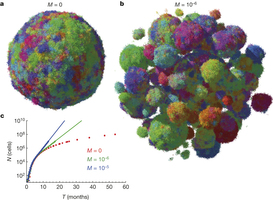
集体所做出的决策往往会减少个人的责任,尤其是偏向于风险更大的决策。许多常见的治疗方案对晚期癌症患者是有毒的和边际效用的。在这种情况下,MDT所做的决策可能会偏向积极治疗,因此往往会疗效不显著,还会引起患者更多痛苦。
肿瘤学家和制药公司所谓的“首选治疗”,通常是次优决策。例如胰腺癌症的“首选治疗”FOLFIRINOX(叶酸、氟尿嘧啶、伊立替康和奥沙利铂)方案,只有一个试验证明了其轻微的有效性,虽然有统计学意义,但对患者是边际效用。MDT应该更多的从病人角度出发思考,而不是“首选治疗”。
关于MDT对指南的依从性还需进一步研究。
许多医生、护士和患者认为MDT所做的决策就是“法律”:必须服从或承担后果。这样下去无论患者还是专家都会失去很多。
谁在做决策?
每一个MDT应明确谁做最后的决策,谁来负责。当然并不是说谁查看了病人谁就要负责。MDT除了相关医生外,应该允许患者的一名代表参与,可以是患者的全科医生或医院的全面人才(有多方面知识和经验的人)。这个代表可以帮助患者把医生的态度和偏好集成到决策过程;通过代表,患者也可以表达自己的意见,再者临床决策的制定过程中,患者意见和专家意见同等重要。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#过度治疗#
110
#BMJ#
104
我们医院也每周开展MDT,但是都在分病人的状态
113
尽管如此mdt还是有继续推广的价值!
134
#多学科#
0
#MDT#
73
一利必有一弊
151