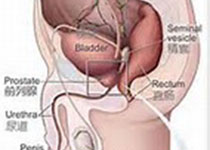
Prostate Cancer P D:前列腺癌初级病灶治疗应该选择哪项技术?
2018-05-20 AlexYang MedSci原创
随着前列腺癌(PCa)局部重点治疗(FT)兴趣的增加,不同治疗形式相关的设备正在增加,包括高强度聚焦超声(HIFU)、冷冻疗法、焦激光烧蚀(FLA)、不可逆电穿透技术(IRE)、血管靶向光动力治疗(VTP)、焦近距离放射疗法(FBT)和烧蚀定向放疗(SABR)。目前,针对病人个体特性选择哪种技术的建议还没有很明确的研究。最近,有研究人员在文献中回顾了不同技术的特殊作用,从而根据病人个体肿瘤特性选择
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
93
#病灶治疗#
58
学习了受益匪浅
104
学习了受益匪浅
121
#ROS#
101
#PRO#
55
学习了.谢谢作者分享!
108