Nature:肺癌第四代TKI有望问世,可以解决AZD9291耐药难题
2016-05-26 萝卜 咚咚癌友圈
靶向药更新换代很快,第一代靶向药主要有:易瑞沙、凯美纳、特罗凯(插播一个好消息:国家有关部门宣布,前面两个药通过国家出面谈判,从下个月开始要降价一半以上了,喜大普奔!) 吃了以上第一代靶向药的患者,平均一年左右就会发生耐药,发生耐药的患者,其中50%左右的病人,都是由于在EGFR这个基因上又产生了一个新的突变,T790M,针对这个突变,目前欧美已经上市了一款“神药”:AZD9291,又能
靶向药更新换代很快,第一代靶向药主要有:易瑞沙、凯美纳、特罗凯(插播一个好消息:国家有关部门宣布,前面两个药通过国家出面谈判,从下个月开始要降价一半以上了,喜大普奔!)
吃了以上第一代靶向药的患者,平均一年左右就会发生耐药,发生耐药的患者,其中50%左右的病人,都是由于在EGFR这个基因上又产生了一个新的突变,T790M,针对这个突变,目前欧美已经上市了一款“神药”:AZD9291,也就是Tagrisso(阿斯利康非小细胞肺癌口服新药Tagrisso获FDA批准上市),又能明显延长生存期差不多一年左右。目前这个药物,国内也有很多类似的产品正在研究,估计这一两年就能上市。
但是,问题来了,不少病友吃了AZD9291,差不多一年多,又耐药了,这可怎么办!!!
自然,逻辑还是一样的,大部分患者是因为EGFR这个基因又产生了更可怕的获得性突变:C797S;但是人类怎么能轻易服输呢,面对变化多端的癌细胞,我们要不断开发新药呀。实际上,这种突变在2015年才刚刚得到证实(附文),同时,一批科学家呼吁针对这种新型获得性突变开展研究!MedSci小编也很兴奋,随着科学进步,新药研发速度也明显提速,从一个靶基因到一个有苗头的化合物发现,只需要一年多时间,这确实令人吃惊!而且,这种小分子化合物,有望通过绿色通道快速通过审批,走上临床(应该在5年左右时间即可!)
今天,世界顶尖学术杂志Nature发表了一篇重磅文章,宣布了一种能够克服AZD9291耐药的新一代靶向药,如果成功上市,应该算第四代靶向药了。
这个神药,长什么样,疗效如何?赶紧分享给大家。
神药长这样,叫做EAI045
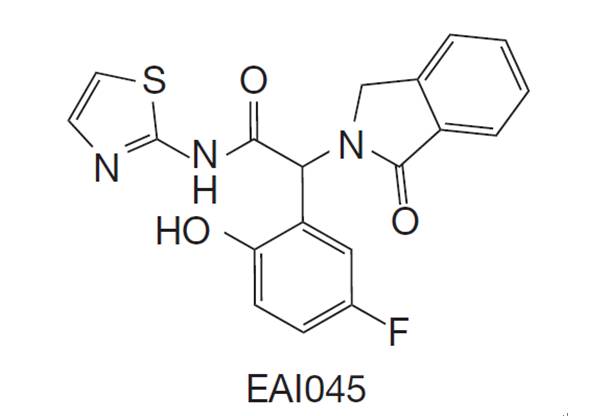
反正药物都是从一堆化合物中筛选和优化出来了,名字是药厂随便取的,反正看不出什么门道。
EAI045和爱必妥联合:小鼠模型中,有效率接近80%
1.用于一代药物耐药,有T790M突变的病人
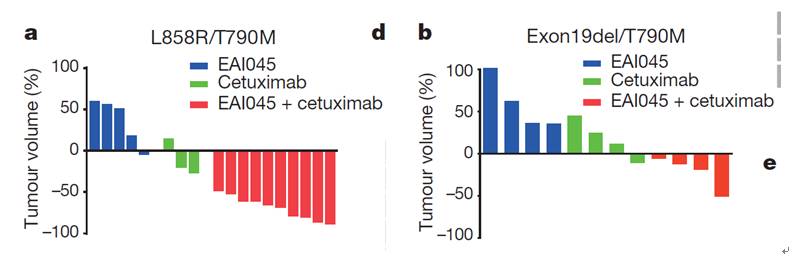
对于这类病人,上文已经提到,已经有神药AZD9291可以吃了,但这个新药和爱必妥连用,似乎也挺好,在小鼠模型中,有效率高达80%左右(图中红色的就是两药联合的病鼠,柱子朝下就代表肿瘤缩小,纵坐标的数字代表肿瘤缩小的比例)。
2. 用于吃AZD9291耐药,有C797S突变的病人

已经有AZD9291了,很多病人并不关心上面两张图,但这张图一定得好好看:这是吃了AZD9291耐药的病人,如果有C797S突变,这个新药和爱必妥连用,在小鼠模型中,有效率高达80%(5只老鼠,4只有效)。
让我们一起期待,这个药物进一步优化,早日上临床试验,早日惠及患者朋友吧!
原始出处:
Yong Jia, Cai-Hong Yun, Eunyoung Park, Dalia Ercan, Mari Manuia, Jose Juarez, Chunxiao Xu, Kevin Rhee, Ting Chen, Haikuo Zhang, Sangeetha Palakurthi, Jaebong Jang, Gerald Lelais, Michael DiDonato, Badry Bursulaya, Pierre-Yves Michellys, Robert Epple, Thomas H. Marsilje, Matthew McNeill, Wenshuo Lu, Jennifer Harris, Steven Bender, Kwok-Kin Wong, Pasi A. Jänne & Michael J. Eck. Overcoming EGFR(T790M) and EGFR(C797S) resistance with mutant-selective allosteric inhibitors.Nature (2016) doi:10.1038/nature17960
相关文献:
Yu HA, Tian SK, Drilon AE, Borsu L, Riely GJ, Arcila ME, Ladanyi M. Acquired Resistance of EGFR-Mutant Lung Cancer to a T790M-Specific EGFR Inhibitor: Emergence of a Third Mutation (C797S) in the EGFR Tyrosine Kinase Domain. JAMA Oncol. 2015 Oct;1(7):982-4. doi: 10.1001/jamaoncol.2015.1066.
Thress KS, Paweletz CP, Felip E, Cho BC, Stetson D, Dougherty B, Lai Z, Markovets A, Vivancos A, Kuang Y, Ercan D, Matthews SE, Cantarini M, Barrett JC, Jänne PA, Oxnard GR. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015 Jun;21(6):560-2.
Song HN, Jung KS, Yoo KH, Cho J, Lee JY, Lim SH, Kim HS, Sun JM, Lee SH, Ahn JS, Park K, Choi YL, Park W, Ahn MJ. Acquired C797S Mutation upon Treatment with a T790M-Specific Third-Generation EGFR Inhibitor (HM61713) in Non-Small Cell Lung Cancer. J Thorac Oncol. 2016 Apr;11(4):e45-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AZD9291#
83
#Nat#
79
#AZ#
75
拜读,好文
131
不错哦继续关注
104
#TKI#
75
用于吃AZD9291耐药,有C797S突变的病人
220
研发迅速!
162
研发迅速!
142