既往研究显示,起源于结肠右侧和左侧的结直肠癌(CRC)在胚胎学、流行病学、遗传学和分子方面存在着差异性。在靶向治疗的时代,目前已被证实原发肿瘤的位置在预测转移性结直肠癌(mCRC)的治疗反应和预后方面发挥着重要作用。
左侧mCRC患者(肿瘤起源于脾曲、降结肠、乙状结肠、直肠乙状结肠连接处,有时甚至是直肠)已被证实比右侧mCRC患者(肿瘤起源于盲肠、升结肠、肝曲和横结肠)具有更好的生存获益。
此外,原发肿瘤的位置也决定了靶向治疗在治疗mCRC中的疗效。就mCRC而言,直肠在先前的试验和研究中通常被归类为左侧结肠的一部分,并根据ESMO和NCCN指南中描述的相同治疗策略进行治疗。
根据最新的ESMO指南,直肠癌主要分为高、中、低位直肠癌(分别距肛缘>10-15、≥5-10和<5 cm)。在临床上,转移性直肠癌通常被认为是左侧结肠癌的一个子集。然而,既往的研究指出,高位和中/低位直肠癌之间存在着异质性。
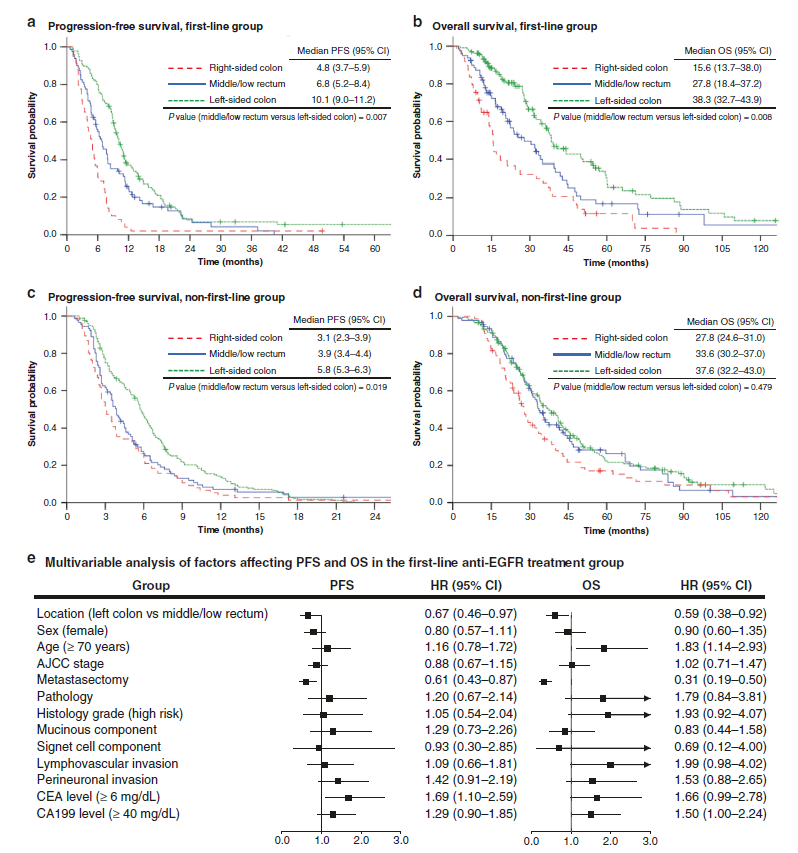
患者的无进展生存期和总生存期
该研究旨在分析抗EGFR(表皮生长因子受体)治疗中/低位直肠癌和左侧结肠癌的疗效。研究人员共招募了609名接受抗EGFR治疗的转移性结直肠癌患者。根据患者原发肿瘤的位置分为以下几组:右侧结肠癌、左侧结肠癌或中/低位直肠癌。研究人员主要分析了一线和非一线抗EGFR治疗策略的疗效。
结果显示,在一线抗EGFR治疗中,中/低位直肠癌患者的无进展生存期、总生存期和总缓解率(分别为6.8个月、27.8个月和43%)显著低于左侧结肠癌患者(分别为10.1个月、38.3个月和66%)。在非一线抗EGFR治疗中也发现了类似的结果。TCGA(癌症基因组图谱)分析显示,直肠癌呈现遗传异质性,且与左侧和右侧结肠癌具有相似的特征。
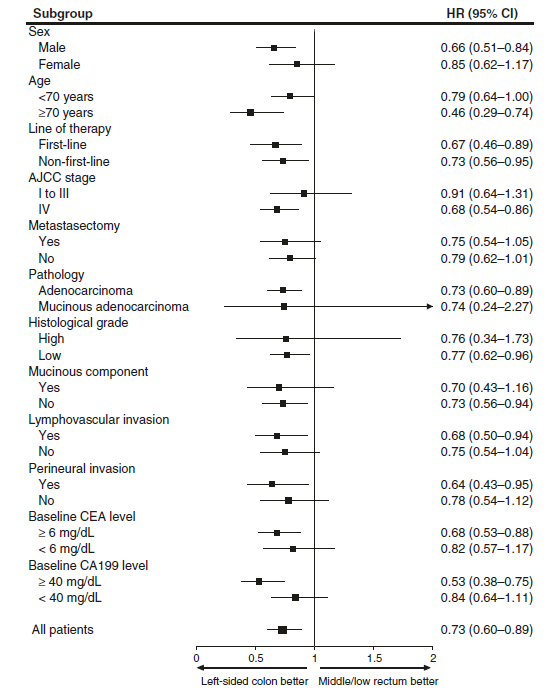
不同亚组患者的无进展生存期森林图
总而言之,该研究结果揭示,抗EGFR治疗对转移性中/低位直肠癌的疗效低于左侧结肠癌。
原始出处:
Lee, KH., Chen, WS., Jiang, JK. et al. The efficacy of anti-EGFR therapy in treating metastatic colorectal cancer differs between the middle/low rectum and the left-sided colon. Br J Cancer (29 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#GFR#
81
好好学习天天向上
0
学习了
102
学习了
107
学习
103
谢谢梅斯提供这么好的信息,学到很多
81
学习了,谢谢分享
66