呼吸科经典病例——肺放线菌病
2017-11-19 MedSci MedSci原创
放线菌常寄生于人体口腔黏膜、牙龈、扁桃体、结肠等处,平时相安无事,当机体抵抗力下降时可通过口腔分泌物入侵呼吸道,从而导致肺部实质病变。放线菌病因发病率低,故易被误诊,需注意。病史:患者为一55岁女性,47岁时曾行右肺中叶切除术,术后病理诊断为肺结核,术后三联抗结核治疗3个月,有2型糖尿病史4年长期服药治疗,具体不详。 者6年前开始无诱因间断出现咳嗽、咳痰、痰中带血丝,偶有低热

放线菌常寄生于人体口腔黏膜、牙龈、扁桃体、结肠等处,平时相安无事,当机体抵抗力下降时可通过口腔分泌物入侵呼吸道,从而导致肺部实质病变。放线菌病因发病率低,故易被误诊,需注意。
病史:
患者为一55岁女性,47岁时曾行右肺中叶切除术,术后病理诊断为肺结核,术后三联抗结核治疗3个月,有2型糖尿病史4年长期服药治疗,具体不详。
者6年前开始无诱因间断出现咳嗽、咳痰、痰中带血丝,偶有低热,给予"抗生素"治疗2周左右症状可缓解,每年发病1~2次。
20天前再次出现发热、咳嗽及咳痰,体温高达39 ℃,伴轻度呼吸困难。门诊查外周血白细胞计数为14.2×10^9/L ,中性粒细胞百分率为0.85,血红蛋白为156 g/L,血小板为240×10^9/L, ESR为18 mm/1h,C反应蛋白为57 mg/L。
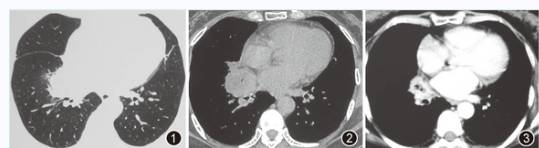
胸部CT平扫示右肺门肿块,直径约4.5 cm,考虑肺癌或肺脓肿可能性大(图1,图2)。给予"盐酸莫西沙星"0.4 g/d静脉滴注,7天后体温降至正常,14 天后复查胸部CT示右肺门肿物明显缩小(图3),为进一步诊治而入我院。
查体:
患者自动体位,精神萎靡,神志清楚、查体合作,皮肤黏膜未见黄染及出血点,浅表淋巴结未及肿大。头颈无异常。胸廓无畸形。左肺呼吸音清,右肺可闻及局限性干啰音,心律齐,无杂音。腹平软,无压痛,肝脾肋下未及。脊柱四肢未见异常。
辅助检查:
支气管镜检查示:右肺中叶和下叶黏膜充血水肿,管腔狭窄(图4)

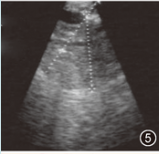
支气管镜内超声:在右肺中下叶间嵴外可探及直径为1.97 cm的软组织肿块(图5)
透壁肺活检病理:可见炎性肉芽组织及坏死渗出,细菌菌团形成,未见肿瘤细胞
治疗1个月后复查胸部CT: 右下肺病灶进一步吸收(图6)

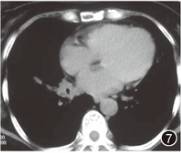
2个月后查胸部CT 示:右下肺近肺门处肿物及斑片状渗出影(图7)
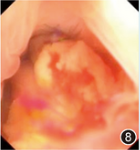
支气管镜复查:右肺中叶支气管被黄色颗粒样物完全阻塞(图8)
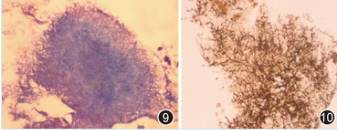
活检病理:革兰染色示为硫磺颗粒,周围可见直径为1 μm、呈放射状生长的菌丝,革兰和六胺银染色阳性(图9,图10)
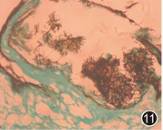
复检第1次透壁肺活检病理:可见同种形态致病菌(图11)
外院专科鉴定:放线菌
其他:多次痰涂片抗酸染色均阴性、痰培养、PPD试验、结核抗体、支原体、衣原体及军团菌抗体均阴性、血清CA19-9 87.6 U/ml 正常值<37 U/ml、过碘酸雪夫染色、抗酸及弱抗酸染色均阴性
简要解析:
肺放线菌病是由放线菌感染引起的一种慢性化脓性肺部疾病,发病率较低,临床医生对该病认识不足,易将其误诊为肺真菌病、肺结核、肺脓肿及肺癌等。即使高度怀疑本病的患者,也很难取得微生物学证据。本例患者在病程伊始也被误诊为肺癌和肺脓肿。
肺放线菌病的确诊依赖于病理学或微生物学,在咳出物涂片找到典型"硫磺颗粒"或在肺活检组织内找到放线菌即可诊断。外科手术和支气管镜检查是重要的活检手段。支气管镜下常表现为黄色颗粒样物阻塞管腔(如本例患者),该物质即为"硫磺颗粒",色黄质硬,核心由菌丝缠结而成,菌丝向四周放射状排列,因此得名放线菌。放线菌菌丝直径约1 μm,细长无分支,革兰和六胺银染色阳性,过碘酸雪夫染色及抗酸、弱抗酸染色阴性,借此可与奴卡菌、真菌、结核菌等鉴别。由于放线菌可为正常人口腔内的定植菌,因此痰培养阳性不能确诊。
肺放线菌病可形成肺脓肿并产生"硫磺颗粒",病灶内血供极差,且常伴有局部支气管引流不畅,因此治疗需选用敏感的抗生素足量、长疗程治疗,疗程至少6~12个月。青霉素类、四环素类、大环内酯类抗生素大多有效,而硝基咪唑类、氨基糖甙类和喹诺酮类一般无效。文献报道,放线菌对新型氟喹诺酮类药物盐酸莫西沙星敏感,本患者应用盐酸莫西沙星初始治疗有效也证实了上述观点,但由于疗程较短而致复发。药物疗效不佳或不能耐受者可行外科手术切除病灶。
更多点评分析,趣味的学习,详情尽在梅斯医生上,您可以在这里体验模拟诊疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#放线菌#
81
学习学习学习
107
不错的文章值得推荐!
125
不错的文章值得推荐!
129
不错的文章值得推荐!
117
值得学习
91
不错的文章值得推荐.
83