Cancers:多中心研究探索局部晚期 Merkel细胞癌的治疗、预后以及相关因素
2022-01-19 yd2015 MedSci原创
该研究分析局部晚期MCC的治疗、预后以及相关因素,建议在有经验的团队进行治疗。
Merkel细胞癌(MCC)是一种罕见的、侵袭性的皮肤癌,复发风险高,预后差。局部晚期MCC的治疗包括手术和放射治疗。为了分析现实生活中的治疗模式和临床结果,来自波兰的团队开展了回顾性研究,对4个肿瘤中心的161名MCC患者进行了回顾性分析。相关结果发表在Cancers杂志上。
纳入的161例患者中,中位年龄72岁(30-94岁),70岁以上占55.9%,男性占49.7%。大约77.6%的患者有其他合并症,其中高血压是最常见的。原发部位以下肢(32.9%)、上肢(29.2%)、头颈部(29.2%)最为常见。26.9%的患者在诊断时发现淋巴结(LN)受累。
161例患者接受了治疗,其中96.9%的患者接受了手术,联合或不联合围手术期治疗,而3.1%的患者仅接受了放疗。手术切缘阴性(R0)的患者为55.2% (85),R1、R2和未知的患者分别为27.9%(43)、0.6%(1)和13.6%(21)。38%(57/150)的患者在原发肿瘤切除后进行了前哨淋巴结活检(SLNB), 10.5%(6)的患者活检阳性。总的来说,26.7%(43)的以治疗为目的的患者进行了淋巴结清扫(LND),其中83.7%(36)为阳性。
156例接受治愈性手术的患者中有81例接受了围手术期治疗(51.9%)。其中化疗17例占21%,放疗70例占86.4%。
中位随访2.3年(95% CI 1.97 2.64年),40.4%(65例)患者复发,局部复发36.6%(59例),远处转移12.4%(20例)。中位DFS未达到,而1年、2年和5年DFS率分别为66%、57%和55%。中位局部无复发生存期(LRFS)和远处无复发生存期(DMFS)未达到。1年、2年和5年LRFS分别为69%、61%和59%,而DMFS分别为92%、86%和86%。
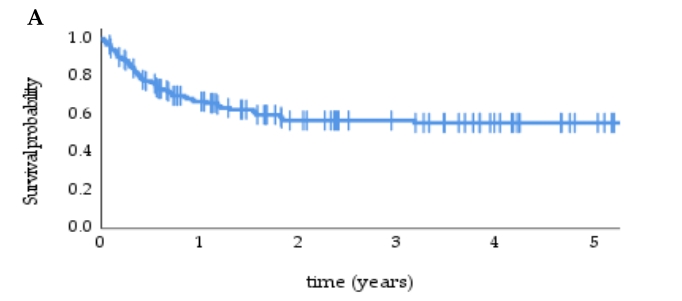
多变量Cox回归模型,显著的负面因素包括:男性(HR 1.42, 95%CI1.06 - 3.01),淋巴结受累(HR 5.41, 95%CI 2.39 - 12.26),无临床淋巴结转移患者同时无SLNB (HR 5.45, 95%CI 2.41 - 12.3),无围手术期放疗(HR 2.19, 95% CI 1.29 - 3.75)。
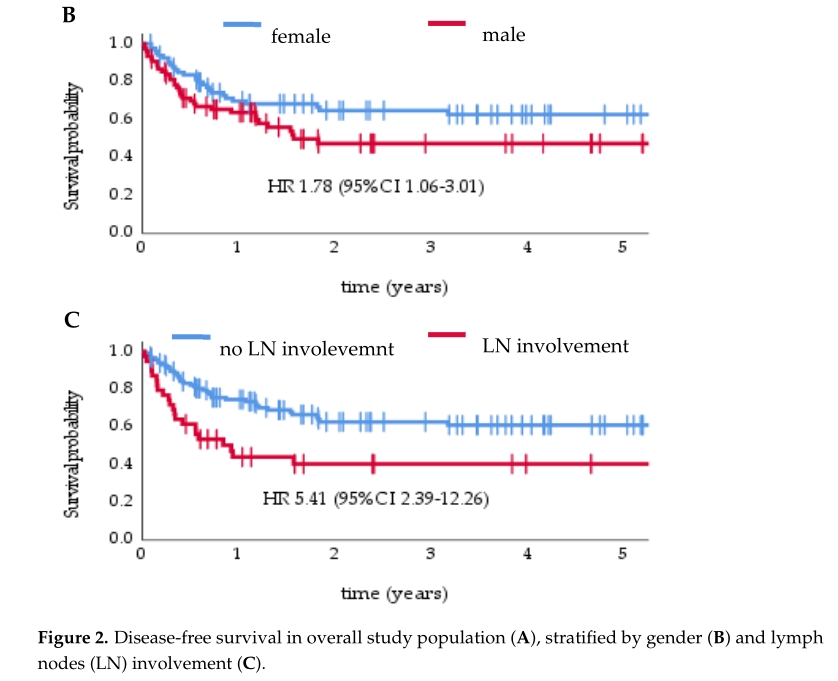
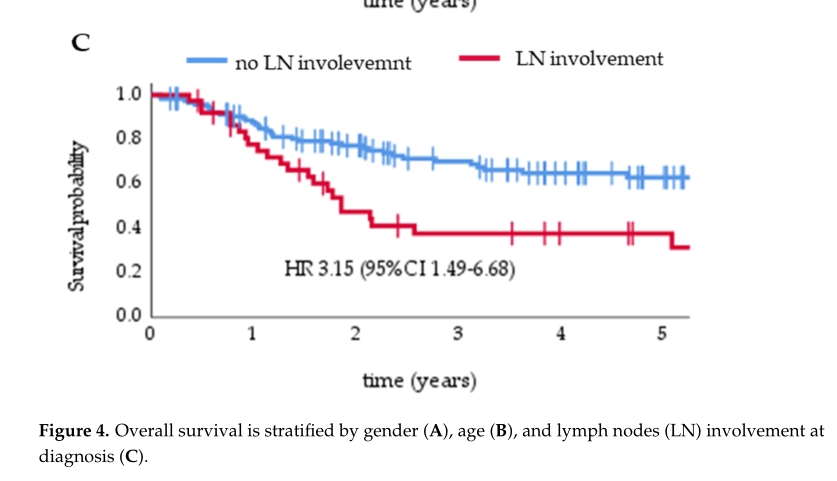
中位OS为6.8年(95% CI 3.56 10.03), 1年、2年和5年OS分别为85%、70%和55%。
多变量Cox回归模型中,显著负向因素包括:男性(HR 1.95, 95% CI 1.16 3.27),≧70岁(HR 2.0, 95% CI 1.15 3.48),淋巴结受累(HR 3.15, 95% CI 1.49 6.68),无临床淋巴结转移患者同时无SLNB (HR 2.30, 95% CI 1.10 4.82)。

综上,该研究分析局部晚期MCC的治疗、预后以及相关因素,建议在有经验的团队进行治疗。
原始出处:
Dudzisz-Sledz, M.; Sobczuk, P.; Kozak, K.; Switaj, T.; Kosela-Paterczyk, H.; Czarnecka, A.M.; Falkowski, S.; Rogala, P.; Morysinski, T.; Spalek, M.J.; et al. Treatment of Locally Advanced Merkel Cell Carcinoma—A Multi-Center Study. Cancers 2022, 14, 422. https://doi.org/10.3390/ cancers14020422
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#细胞癌#
52
#ERK#
58
#局部晚期#
48
#ERS#
47
#多中心#
48
#多中心研究#
65
#局部#
43
#相关因素#
50