Lancet Haematol:早期识别血管内皮细胞病变并减轻其进展或可改善COVID-19患者的结局
2021-04-26 MedSci原创 MedSci原创
严重急性呼吸系统综合征冠状病毒2发病机制的一个重要特征是COVID-19相关的凝血病,其特点是血栓性和微血管并发症增加。既往研究表明,内皮细胞损伤在COVID-19相关的凝血病中发挥作用。近日,为了确
严重急性呼吸系统综合征冠状病毒2发病机制的一个重要特征是COVID-19相关的凝血病,其特点是血栓性和微血管并发症增加。既往研究表明,内皮细胞损伤在COVID-19相关的凝血病中发挥作用。近日,为了确定内皮细胞病变是否参与COVID-19相关的凝血病发病机制,研究评估了COVID-19入院的重症和非重症患者的内皮细胞和血小板激活标志物,研究结果已发表于Lancet Haematol。
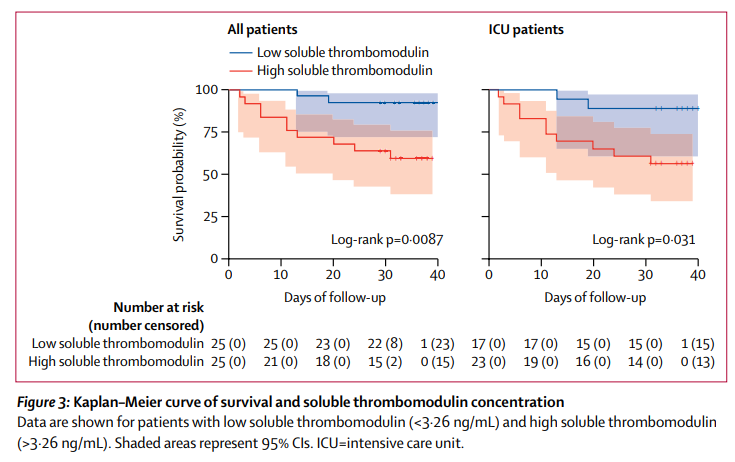
在这项单中心横断面研究中,研究人员纳入了COVID-19的住院成年(≥18岁)患者,同时招募无症状、非住院的参与者作为对照组。评估了内皮细胞和血小板激活的标志物,包括Von Willebrand Factor(VWF)抗原、可溶性血栓调节蛋白、可溶性P-选择素和可溶性CD40配体,以及凝血因子、内源性抗凝血剂和纤维蛋白溶解酶。比较了ICU患者、非ICU患者和对照组每种标志物的水平。评估这些实验室结果与临床结果之间的相关性,包括出院和死亡率。采用Kaplan-Meier分析法,进一步探讨生化标志物与生存的关系。
2020年4月13日至4月24日,研究共纳入了68名COVID-19患者,包括48名ICU和20名非ICU患者,以及13名非住院、无症状的对照组。分析结果显示,与非ICU患者相比,ICU患者的内皮细胞和血小板激活的标志物明显升高,包括VWF抗原(ICU患者平均565%[SD 199]vs非ICU患者平均278%[133];P<0.0001)和可溶性P-选择素(15.9 ng/ml[4-8]vs 11-2 ng/ml[3-1];P=0.0014)。在20名非ICU患者中,16名(80%)患者的VWF抗原浓度升高到正常范围以上。所有患者的死亡率与VWF抗原(r=0-38;p=0-0022)和可溶性血栓调节蛋白(r=0-38;p=0-0078)的水平密切相关。Kaplan-Meier分析显示,可溶性血栓调节蛋白浓度大于3.26ng/mL 与较低的出院率(25名低浓度患者中有22名[88%]vs. 25名高浓度患者中有13名[52%];P=0-0050)和较低的生存相关(危险比5.9,95%CI 1.9-18.4;P=0.0087)。
综上所述,研究结果表明,COVID-19患者存在内皮细胞病变问题,且内皮细胞病变可能与危重病和死亡有关。早期识别内皮病变和减轻其进展可能会改善COVID-19患者的结局。
原始出处:
George Goshua, et al., Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020 Aug;7(8):e575-e582. doi: 10.1016/S2352-3026(20)30216-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
55
#HAE#
54
#血管内皮细胞#
87
#COVID-19患者#
61
#EMA#
61
不错
79
非常的棒
77
顶刊就是不一样,质量很高,内容精彩!学到很多
60