Clin Gastroenterology H: 自身免疫性肝炎会增加患者死亡的风险
2021-11-23 MedSci原创 MedSci原创
自身免疫性肝病(autoimmune liver disease, ALD)是因体内免疫功能紊乱引起的一组特殊类型的慢性肝病,包括自身免疫性肝炎(autoimmune hepatitis ,AIH)。
自身免疫性肝炎 (AIH) 是一种慢性炎症性肝病,可进展为肝硬化和肝功能衰竭,但早期关于AIH是否会导致死亡风险增加的研究的结论是互相矛盾的。关于肝硬化是否影响 AIH 死亡率的数据也存在差异。与一般人群相比,自身免疫性肝炎(AIH)患者的预后尚不清楚。因此,本项研究旨在探究自身免疫性肝炎是否会增加患者死亡的风险。

本项研究是一项是1969年至2017年在瑞典进行的基于全国性人群的队列研究,研究对象为6,016名AIH成人和28,146名匹配的健康对照人群。AIH的定义是AIH的医学诊断加上病理学的肝活检证实。通过Cox回归,研究人员估计了AIHy引起的总体和特定原因死亡的风险比 (HR)。另外研究人员还观察了所有患者的主要死亡结局的差异。

研究结果显示在随访期间,有3,185名AIH患者死亡(41.4/1000人年),而健康对照g个体仅为10,477 人(21.9/1000 人年)。 AIH个体的10年累积死亡发生率为 32.3% (95%CI = 31.1-33.6),健康对照个体为14.1% (95%CI = 13.7-14.5),AIH的死亡率明显处于较高水平。活检发现肝硬化的AIH个体具有更高的死亡风险(HR = 4.55;95%CI = 3.95-5.25),而纤维化、无纤维化的炎症或坏死患者之间的死亡率没有差异。门脉高压和胆汁淤积性肝病的合并症也与死亡风险增加有关。AIH与心血管疾病(HR = 1.27;95%CI = 1.15-1.40)、肝脏疾病(HR = 66.24;95%CI = 48.19-91.03)和肝外恶性肿瘤(HR = 1.69;95%CI = 1.51-1.89)的死亡风险增加有关。
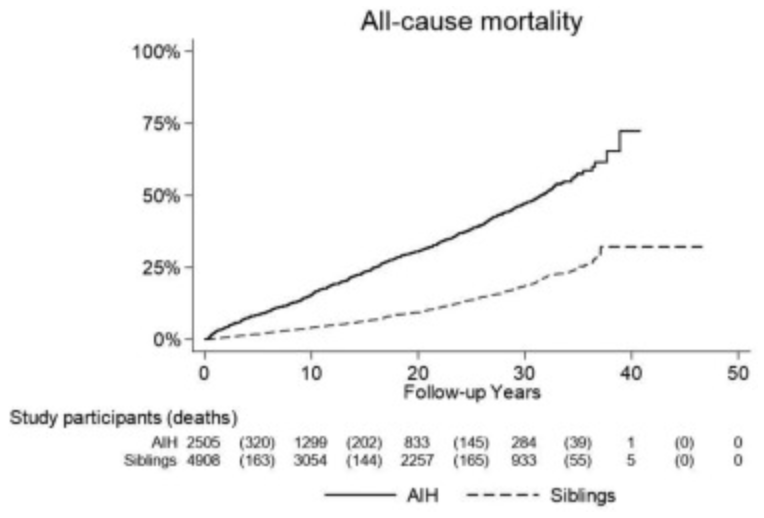
通过本项大样本的人群回顾性队列研究发现AIH会使肝病患者的死亡风险增加2倍左右。肝硬化、门静脉高压症和胆汁淤积性肝病患者的死亡风险特别高。
原始出处 :
Rajani Sharma.et al. Increased Mortality Risk in Autoimmune Hepatitis: A Nationwide Population-Based Cohort Study With Histopathology. Clinical Gastroenterology Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
77
#AST#
62
#患者死亡#
75
#Gastroenterol#
104
#Gastroenterology#
74