JCEM:糖尿病患者肌少症的患病率和危险因素
2021-12-24 从医路漫漫 MedSci原创
糖尿病患者由于血糖控制不良可能会出现多种并发症。糖尿病肌少症是近年来备受关注的糖尿病并发症。肌少症认为与糖尿病患者的胰岛素抵抗和氧化应激有关。导致肌肉力量和肌肉质量下降,以及肌肉萎缩。
糖尿病患者由于血糖控制不良可能会出现多种并发症。糖尿病肌少症是近年来备受关注的糖尿病并发症。肌少症认为与糖尿病患者的胰岛素抵抗和氧化应激有关。导致肌肉力量和肌肉质量下降,以及肌肉萎缩。肌少症在老年人中定义为随着年龄的增长而发生的骨骼肌质量下降、肌肉力量下降或身体能力下降,糖尿病患者是糖尿病相关肌少症的高危对象。此外,行动缓慢是肌少症的一种表现,而肌少症与2型糖尿病患者的跌倒密切相关。据了解,肌肉质量下降会显著增加这些患者的住院率,导致卧床,从而增加肺部感染的风险,降低老年糖尿病患者的生活质量。因此,积极评估和筛选肌少症患者,以提高其生活质量,减轻国家、社会和家庭的经济负担是非常重要的)。然而,基于不同研究人群(如不同性别和不同年龄组)的研究显示,肌少症的患病率差异很大,在7.2%至31.1%之间。糖尿病患者肌少症的患病率是非糖尿病患者的三倍,且与不良预后相关。本研究的目的是探讨糖尿病患者肌少症的全球流行率和危险因素。
方法:
数据来源:从PubMed、Embase、Web of science、万方、知网、维普和CBM等数据库中鉴定了从成立之日起至2020年11月30日发表的相关研究。我们使用以下文本:“糖尿病/糖尿病糖尿病/ 2型糖尿病2型糖尿病/ Diabet * / 1型糖尿病(T1DM,”“Sarcopenia /肌肉萎缩、肌肉萎缩、肌肉/肌肉力量,”“风险因素/影响因素因素/危险因素有关,”“发病率和患病率/流行病学/频率,这些数据库进行搜索。在中文数据库中,使用相应的中文术语进行搜索。我们也检查了参考书目在检索文章可能适当的研究。
纳入与排除标准:纳入标准如下:(1)研究设计:观察性研究,包括横断面研究和前瞻性/回顾性队列研究;(2)研究参与者:年龄≥18岁,临床诊断糖尿病,诊断标准符合世界卫生组织标准(25),不论性别或糖尿病类型;(3)暴露因素:肌减少症。文献中有明确的诊断骨骼肌减少症的参数,如骨骼肌质量指数(SMI),以及亚洲骨骼肌减少症工作组(AWGS)、EWGSOP和美国国立卫生研究院基金会(FNIH)的标准;(4)结局指标:骨骼肌减少症的发生率;(a)一般因素包括年龄、性别、体重指数(BMI)、内脏脂肪面积(VFA)和吸烟。(b)疾病相关因素包括糖化血红蛋白(HbA1c)、糖尿病持续时间、高敏c反应蛋白(HS-CRP)。(c)与治疗相关的因素包括运动和药物。
研究选择:年龄≥18岁的临床诊断糖尿病患者。性别和糖尿病类型不受限制。
数据提取:数据是由两名审查员使用标准数据收集表格独立提取的。
结果:糖尿病患者肌少症的合并患病率为18% (95% CI,16-20),亚组分析显示,肌肉减少症在男性中比在女性中更普遍,并且在亚洲比在南美洲和大洋洲更普遍。年龄(OR, 1.10)、糖化血红蛋白(OR, 1.16)、内脏脂肪面积(VFA) (OR, 1.03)、糖尿病肾病(OR, 2.54)、糖尿病病程(OR, 1.06)和HS-CRP (OR, 1.33)是糖尿病患者肌少症的危险因素。
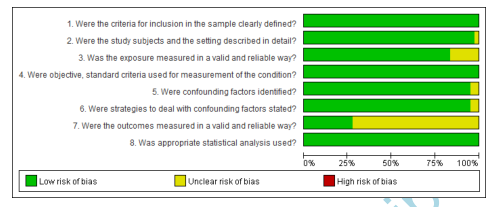
图1 横断面研究的质量评价结果
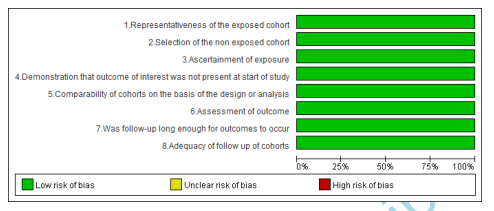
图2 队列研究质量评价结果

图3 糖尿病患者肌少症的总患病率
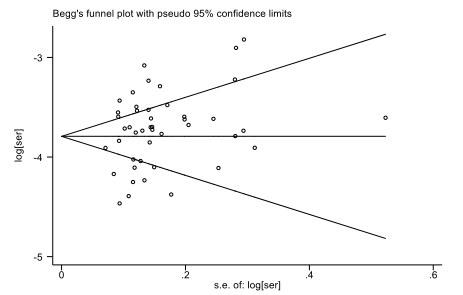
图4 糖尿病患者骨质疏松症总体患病率的发表偏倚

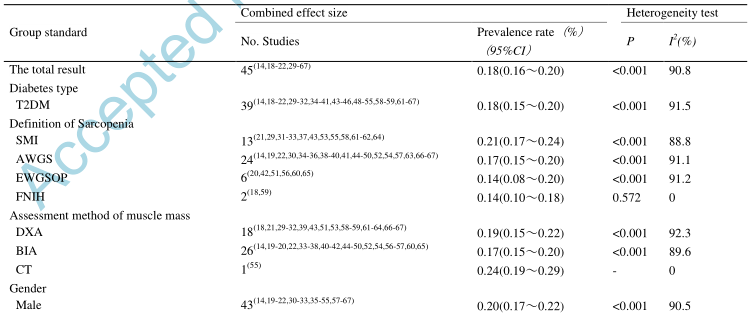
表1糖尿病患者骨质疏松症患病率的亚组分析

表2 糖尿病患者发生骨质疏松症的危险因素分析
结论。肌少症在糖尿病患者中更为普遍。年龄、糖化血红蛋白(HbA1c)、内脏脂肪面积(VFA)、糖尿病肾病、糖尿病持续时间、HS-CRP是可能的危险因素。今后,医护人员不仅要重视对高危人群的早期筛查,还要提供预防信息。
原文出处:
Feng L, Gao Q, Hu K,et al.Prevalence and risk factors of sarcopenia in patients with diabetes: A meta-analysis.J Clin Endocrinol Metab 2021 Dec 14
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCEM#
72
#JCE#
94
进一步学习肌少症,非常棒
92
热门话题
109
点赞
83
#患病率#
97
#糖尿病患者#
63