Oncol Res Treat:乳腺癌新辅助治疗疗效评价指标大盘点
2014-12-23 MedSci MedSci原创
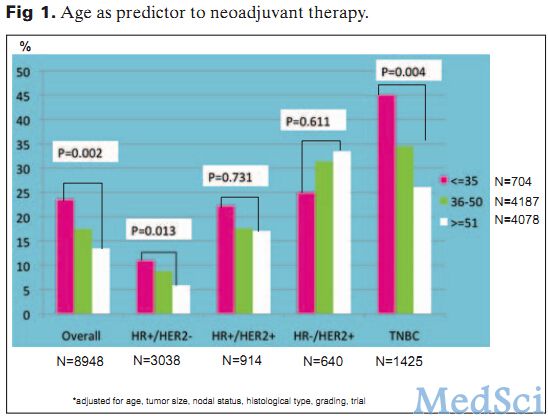
Oncol Res Treat:乳腺癌新辅助治疗疗效评价指标大盘点 新辅助治疗(NAT)已成为一种标准治疗,NAT后达到病理完全缓解(PCR)预示着较好的长期预后(DFS、OS),但仍有40-880%患者无法达到PCR,那么PCR与什么因素有关呢?本文将告诉你。 年龄:年龄是达到PCR的重要预测因素(FIG1),较年轻的患者较年龄大的患者更容易达到PCR(尤其是TNBC和HR
新辅助治疗(NAT)已成为一种标准治疗,NAT后达到病理完全缓解(PCR)预示着较好的长期预后(DFS、OS),但仍有40-880%患者无法达到PCR,那么PCR与什么因素有关呢?本文将告诉你。
年龄:年龄是达到PCR的重要预测因素(FIG1),较年轻的患者较年龄大的患者更容易达到PCR(尤其是TNBC和HR+/HER2+亚型患者)。
体重指数:BMI和年龄有密切关系,高BMI患者更难达到PCR,而正常BMI患者有最好的DFS和OS。
化疗敏感性:在前2-4周期就对化疗有较好反应的患者较无反应患者有更高的PCR率(22% vs 5%),并且,对较好反应患者强化治疗或者对无反应患者更改治疗方案即使达不到PCR,也将会增加其DFS和OS。
激素受体:HR状态是乳腺癌最重要的标记物,几乎所有临床试验都提示luminl亚型在NAT中没有很好的疗效,但是却有很好预后,而雄激素受体(AR+)是DFS和OS的独立预后因素,AR+肿瘤较AR-肿瘤PCR率低。而对于缺少标记的TNBC来说,其PCR率与AR状态无关。
肿瘤级别:肿瘤级别被认为是PCR的独立预测因素(三级被认为最容易达到PCR),然而最容易到达PCR的是年龄<40岁的未分化癌。
Ki-67:对于不同分子亚型肿瘤,反映扩增的标记物Ki-67在NAT反应和预后都有很好的预测价值。目前对于Ki-67在反应预后的临界值上仍有争议,对于激素受体阳性肿瘤,Ki-67临界值14%将其作为预后较好的(luminalA亚型)和预后较差(luminalB亚型)的标准。
基因组等级指数(GGI):GGI被认为较传统的组织分级评价标准能更好的反映预后及更好的对肿瘤分类。对于HER2-肿瘤,高GGI被认为与较好的化疗反映独立且显著相关。
复发评分(RS):RS将21个基因用于量化雌激素受体(+),淋巴结(-)患者复发风险,同时RS还与PCR有关。高RS患者复发风险较高。
肿瘤浸润淋巴细胞(TILs):TILs在大量文献中认为与PCR相关。TILs可分为瘤内、基质、淋巴细胞为主的乳腺癌(LPBC),TILs可持续预测NAT的反应(FIG2),LPBC与非LPBC相比有更高的PCR率。

三阴性乳腺癌(TNBC):TNBC可被分为6个不同亚组,BLBC1型有较好的PCR率(52%),而BLBC2型和luminalAR型PCR最低(0%、10%)。
BRCA突变:BRCA1突变患者较BRCA2携带者和无携带者有更高的PCR率。
HER(+):由于靶向治疗的进展及其与化疗的联合运用,HER+患者PCR率持续上升,但两者靶向治疗联合运用与单药相比甚至可使PCR达到51.3%。
P95HER2(P95):P95存在于HER2的C端,是一种新型标记物,可预测HER2+患者NAT的疗效,GeparQuattro研究表明P95(+)患者较P95(-)患者在化疗后行靶向治疗有更好的PCR率。
PIK3CA基因:PIK3CA基因是乳腺癌位列第二突变的基因,作为另一个新型标记物,20.8%HER2+肿瘤存在PIK3CA突变,对于HER2+患者,PIK3CA突变患者有较低的PCR率,此外有PIK3CA突变的HER2+/HR+患者PCR率也只有6.3%。
以上是可预测新辅助治疗效果的因素,治疗效果与其PCR有关,了解与NAT有关的疗效因素可预测疗效,以便对特定患者采取个性化治疗,提高患者PCR率,达到长期生存的目的。
原文出处:
Loibl, S., et al., Predictive factors for response to neoadjuvant therapy in breast cancer. Oncol Res Treat, 2014. 37(10): p. 563-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
47
#TREAT#
64
#新辅助#
45
越来越难看到Os
134
#疗效评价#
75
#评价#
54