J Crohns Colitis:肉吃的越多,溃疡性结肠炎风险越高!
2022-04-16 Nebula MedSci原创
高溃疡性结肠炎风险人群或可适当减少肉类摄入以降低发病风险
炎症性肠病(IBD,包括克罗恩病和溃疡性结肠炎)的发病率日益增加,该趋势提示环境因素在IBD病例过程中可能具有重要作用。工业化与许多生活方式的改变有关,包括城市化、医疗保健、抗生素的广泛使用、暴露于不同类型的环境污染、缺乏体育活动和西式饮食。
本研究旨在探索蛋白质摄入和炎性肠病风险的相关性。
纳入了来自欧洲8个国家的413594位受试者。通过食物频率问卷收集基线时的膳食数据。膳食数据经过校准,以纠正与每个国家特定问卷相关的测量错误。采用Cox比例风险模型评估蛋白质(总的、动物性和植物性)或动物蛋白食物来源于IBD风险的相关性。
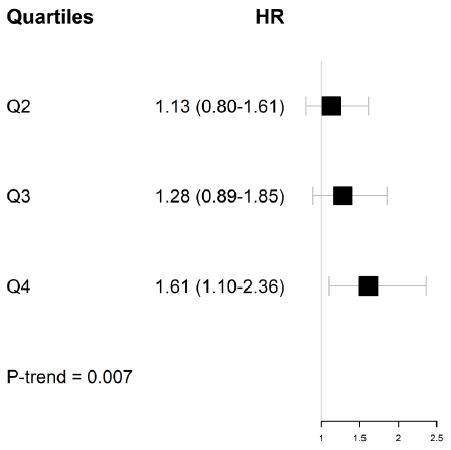
肉类摄入量与溃疡性结肠炎风险的相关性
平均随访了16年后,确诊了177例克罗恩病(CD)和418例溃疡性结肠炎。总蛋白、动物或植物性蛋白摄入量与克罗恩病或溃疡性结肠炎风险之间没有关联。总肉类和红肉摄入量与溃疡性结肠炎风险相关(最高四分位与最低四分位人群相比的风险比[HR] 1.40,p=0.01)。动物蛋白的其他食物来源(加工肉类、鱼类、贝类、蛋类、家禽)与溃疡性结肠炎风险无相关性。此外,动物蛋白的任何食物来源均与克罗恩病风险无相关性。
综上所述,该研究结果显示,肉类和红肉摄取量与溃疡性结肠炎风险相关,即摄取量越大,患病风险越高;提示高溃疡性结肠炎风险人群或可适当减少肉类摄入以降低发病风险。
原始出处:
Dong Catherine,Chan Simon S M,Jantchou Prevost et al. Meat intake is associated with a higher risk of ulcerative colitis in a large European prospective cohort study.[J] .J Crohns Colitis, 2022, https://doi.org/10.1093/ecco-jcc/jjac054.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#溃疡性#
55
#Crohn#
46
#CRO#
0
#结肠炎##溃疡性结肠炎#
79
学习了,谢谢分享
59
学习
59
#colitis#
60