J Crohns Colitis:维多珠单抗治疗溃疡性结肠炎或克罗恩病小儿患者的疗效与安全性
2022-03-22 Nebula MedSci原创
维多珠单抗治疗小儿炎性肠病的药代动力学、安全性和有效性
维多珠单抗(Vedolizumab)是一种整合素受体拮抗剂,是第一个也是目前唯一一个专门针对肠道炎症信号通路的药物。现已获批用于治疗对传统治疗或肿瘤坏死因子α(TNFα)抑制剂应答不充分、失应答或不耐受的中重度活动性溃疡性结肠炎(UC)和克罗恩病(CD)成年患者。
但迄今为止,尚无维多珠单抗在儿童炎症性肠病(IBD)中的系统药代动力学(PK)数据。本文报告了一项名为HUBBLE的2期临床试验的结果,该试验评估了静脉注射维多珠单抗治疗小儿炎性肠病的药代动力学、安全性和有效性。
研究流程
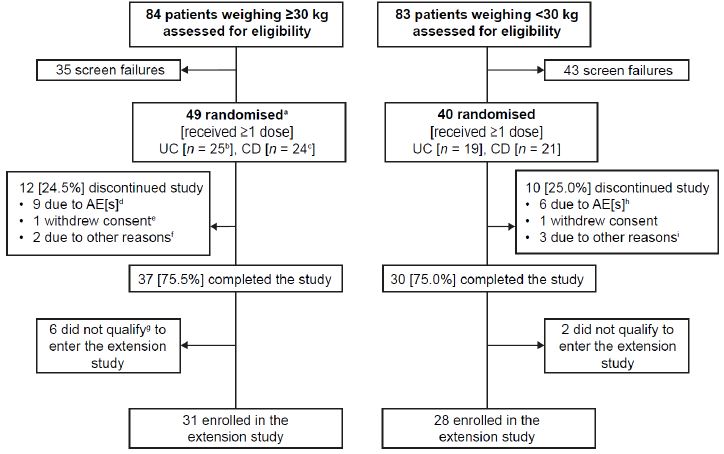
招募了2-17岁的体重≥10 kg 的中重度溃疡性结肠炎或克罗恩病患儿,根据体重随机接受低剂量或大剂量维多珠单抗(≥30 kg:150或200 mg;<30 kg:100或200 mg;第1天,第2周、第6周和第14周)。第14周时评估患儿的药代动力学、临床反应和暴露反应相关性。同时还评估了安全性和免疫原性。
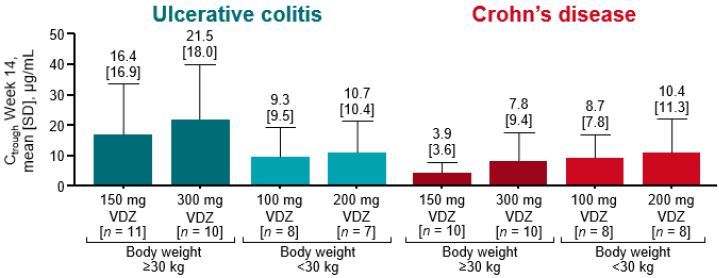
各组第14周时的药物谷浓度
共招募了49位体重≥30 kg(UC 25位,CD 24位)和40位体重<30 kg(UC 19位,CD 21位)的患儿,基线平均年龄分布是13.5岁和7.6岁。在每个适应症和剂量组,浓度曲线下面积和平均浓度由低剂量到高剂量几乎都增加了2倍上下;与低剂量组相比,高剂量组的药物谷浓度都明显更高。在第14周时,在两个体重队列中,UC组和CD组获得临床反应的患儿率分别是40.0%-69.2%和33.3%-63.6%。获得临床反应的溃疡性结肠炎患儿的药物谷浓度一般都高于无应答者,但在克罗恩患儿中未观察到这种趋势。
治疗相关不良事件
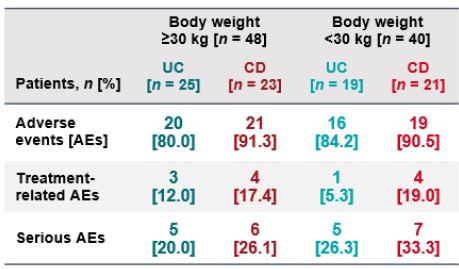
14%(12/88)的患儿发生了治疗相关不良事件,6.8%(6/88)的患儿产生了抗药物抗体。
总而言之,维多珠单抗的暴露量以近似剂量比例的方式增加。在该研究队列中未观察到明确的剂量-反应关系。无新的安全性问题出现。
原始出处:
Hyams Jeffrey S,Turner Dan,Cohen Stanley A et al. Pharmacokinetics, Safety, and Efficacy of Intravenous Vedolizumab in Paediatric Patients with Ulcerative Colitis or Crohn's Disease: Results from the Phase 2 HUBBLE Study.[J] .J Crohns Colitis, 2022, https://doi.org/10.1093/ecco-jcc/jjac036
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CRO#
0
#疗效与安全性#
64
#溃疡性#
69
#Crohn#
65
#治疗溃疡性结肠炎#
64
#colitis#
72