Prostate Cancer P D:未治疗转移前列腺癌前期化疗的生存率研究
2020-09-17 AlexYang MedSci原创
基于临床试验数据,前期化疗可延长转移性、激素敏感性前列腺癌(mHSPC)男性的总生存。最近,有研究人员在一个真实世界的队列中评估了前期化疗与mHSPC男性总生存之间的关联。
基于临床试验数据,前期化疗可延长转移性、激素敏感性前列腺癌(mHSPC)男性的总生存。最近,有研究人员在一个真实世界的队列中评估了前期化疗与mHSPC男性总生存之间的关联。
研究人员对美国一个大型全国性癌症数据库的新发、未接受治疗的转移性前列腺癌男性进行了一项回顾性队列研究(2014-2015年)。前期化疗组的男性为在诊断后4个月内接受了化疗(n=1033,28%),对照组为没有化疗或在诊断后12个月以上接受化疗(n=2704,72%)。研究发现,经过中位值为23个月的随访,前期化疗组的总生存期中值为35.7个月,对照组为32.5个月(对数秩P<0.001)。调整患者和临床变量后,前期化疗与更长的总生存期相关(风险比0.78,95%CI 0.68-0.89,p<0.001)。在探索性分析中,前期化疗与总生存期之间的相关性没有因年龄组、种族或并存症数量而产生差异(所有交互作用p>0.2)。
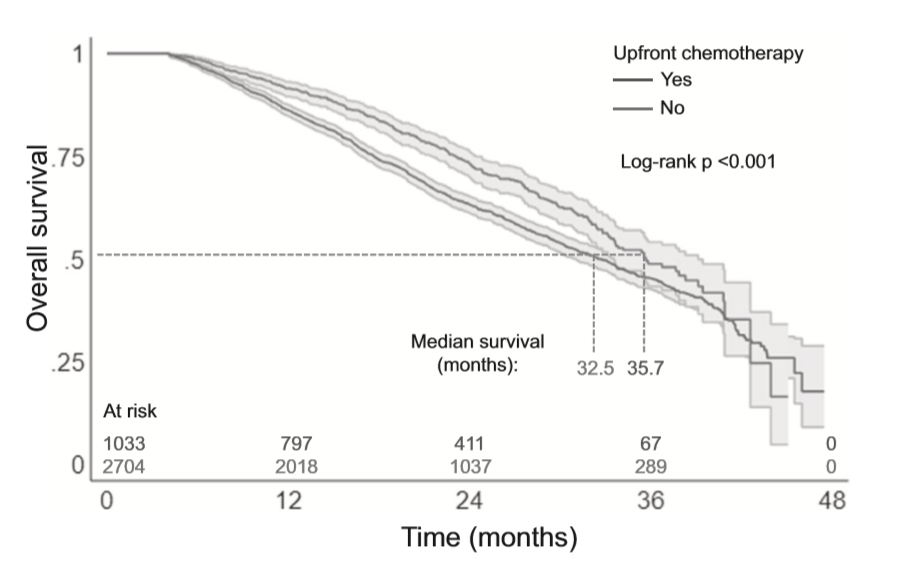
基于前期化疗的总生存Kaplan–Meier生存评估
最后,研究人员指出,在这个真实世界队列中,mHSPC的前期化疗与更长的总生存相关。这些数据支持了对患有mHSPC的男性继续使用化疗;如果患者适合化疗,则可以忽略他们的种族或年龄。研究人员还强调了在临床试验之外评估癌症疗法的重要性,从而阐释在人群中治疗的有效性,而这些疗法可能在临床试验中被低估。
原始出处:
Adam B. Weiner, Oliver S. Ko, Eric V. Li et al. Survival following upfront chemotherapy for treatment-na?ve metastatic prostate cancer: a real-world retrospective cohort study. Prostate Cancer P D. Sep 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
73
#生存率#
73
#ROS#
73
#PRO#
96
学习
155
前列腺癌相关研究,学习了,谢谢梅斯
112