Gastroenterology:麻醉会增加结肠镜检查后并发症风险
2016-03-31 zhaoshuang 译 MedSci原创
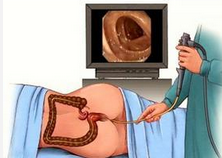
近期有研究者对伴或伴麻醉的结肠镜检查进行了一项研究,发表在Gastroenterology的结果称,伴麻醉的结肠镜检查,其后30天内的并发症风险增加13%(与不伴麻醉的结肠镜检查相比)。尤其是穿孔、出血、腹痛、继发于麻醉的相关并发症和卒中风险增加。研究者呼吁,随着无痛结肠镜检查的广泛应用,临床医师和患者应该对其潜在的风险予以重视。该研究共纳入了3,168,228名40-64岁进行结肠镜检查的人群。
近期有研究者对伴或不伴麻醉的结肠镜检查进行了一项研究,发表在Gastroenterology的结果称,伴麻醉的结肠镜检查,其后30天内的并发症风险增加13%(与不伴麻醉的结肠镜检查相比)。尤其是穿孔、出血、腹痛、继发于麻醉的相关并发症和卒中风险增加。
研究者呼吁,随着无痛结肠镜检查的广泛应用,临床医师和患者应该对其潜在的风险予以重视。
该研究共纳入了3168228名40-64岁进行结肠镜检查的人群。根据有无麻醉将其分组,比较检查后30天内并发症情况。
研究数据显示,整个美国的结肠镜检查中约有34.4%的使用了麻醉,不过不同州和地区的使用率不一致,比如东北和西部地区相比分别为53%和8%(P < .0001)。
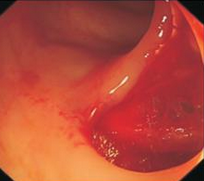
结肠镜检查过程中选择麻醉,则其30天内的并发症风险增加13%(95% CI, 1.12–1.14),尤其是穿孔(OR, 1.07; 95% CI, 1.00–1.15)、出血(OR, 1.28; 95% CI, 1.27–1.30)、腹痛(OR, 1.07; 95% CI, 1.05–1.08)、继发于麻醉的并发症(OR, 1.15; 95% CI, 1.05–1.28)和卒中(OR, 1.04; 95% CI, 1.00–1.08)。此外研究者还观察到,息肉切除术患者的穿孔风险更大(OR = 1.26; 95% CI, 1.09-1.52)。
研究人员总结说:“结肠镜检查所带来的风险并没有在可以接受的范围内,所以随着麻醉的广泛使用,应该充分了解和认识到其背后潜在的风险。”
原始出处:
Wernli KJ, et al. Risks Associated With Anesthesia Services During Colonoscopy.Gastroenterology. 2016;doi:10.1053/j.gastro.2015.12.018.
Risk for complications after colonoscopy increases with anesthesia services.Healio.March 30, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
74
#AST#
74
学习了,平时工作还真没注意到
111
#Gastroenterol#
55
不错哦,会学到很多
98
文章不错,值得拜读
91
#并发#
66
麻醉风险
174
不做无痛?
148
可能是真的
119