JAMA:氧浓度越高越好?危重病人器官功能障碍时怎么选氧浓度?
2021-09-04 MedSci原创 MedSci原创
在多器官功能衰竭危重病人中,与高Pao2正常值目标相比,低Pao2正常值目标的治疗并没有导致器官功能障碍的统计学上的明显减少。
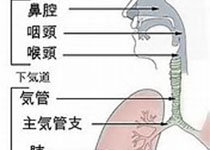
在重症监护室(ICU)中,通常会大量给氧以治疗或预防低氧血症。多年来,氧气被认为具有持续的有利影响。然而,一项使用1999-2006年数据的观察性研究显示,Pao2与死亡率之间呈U型关系-,从而开启了关于危重病人最佳氧合目标的辩论。
高氧血症的潜在负面影响包括肺部毒性,加重缺血/再灌注损伤,以及全身血管收缩导致器官灌注减少,这些影响可能会损害而不是改善组织的氧输送。全身血管收缩可以减少全身炎症反应综合征(SIRS)患者的血管扩张,有利于重新分配器官的血流。
在ICU患者中进行的6项随机临床试验(RCTs)和1项荟萃分析对低氧与高氧目标进行了比较,结果并不一致。其中两项试验和荟萃分析报告了低氧饱和度目标的死亡率降低,而4项试验结果没有差异。此外,一项试验报告了低氧饱和度目标组中肠系膜缺血的发生率增加。
为了确定低正常Pao2目标与高正常目标相比,是否能减少SIRS重症患者的器官功能障碍,来自荷兰阿姆斯特丹心血管科学部、阿姆斯特丹感染和免疫研究所的专家开展了多项随机对照试验,结果发表在近期JAMA杂志上。
研究人员在荷兰的4个重症监护室进行多中心随机临床试验。入选时间为2015年2月至2018年10月,随访结束时间为2019年1月,包括有2个以上器官损害且预计住院时间超过48小时的入院成年患者。共有9925名患者接受了资格筛选,其中574人符合入组标准并被随机分配。
目标Pao2范围为8至12千帕(低-正常,n = 205)和14至18千帕(高-正常,n = 195)。主要终点是SOFARANK,这是一个非呼吸器官衰竭的排名结果,由顺序器官衰竭评估(SOFA)得分中的非呼吸部分量化,在前14个研究日中进行汇总。参与者从器官衰竭改善最快(最低分)到器官衰竭恶化或死亡(最高分)进行排名。次要终点是机械通气时间、院内死亡率和低氧测量。
在574名随机入组的患者中,400名(70%)在24小时内入组(中位年龄,68岁;140名女性[35%]),所有患者都完成了试验。各组之间的Pao2中位数差异为-1.93千帕(95%CI,-2.12~-1.74;P < .001)。
在重症监护室第1至15天活着的病人按治疗组的Pao2值
结果显示,低正常Pao2组的SOFARANK评分中位数为-35分,高正常Pao2组为-40分(中位数差异=10,95%CI:0-21)。机械通气的中位时间(3.4天 vs 3.1天;中位差异=-0.15,95%CI:-0.88~0.47)和院内死亡率(32% vs 31%;OR=1.04,95%CI:0.67-1.63)没有显著差异。
同时,轻度缺氧在低正常值组更经常发生(1.9% vs 1.2%;中位数差异=0.73,95% CI:0.30- 1.20)。低正常Pao2组有20名患者(10%)和高正常Pao2组有21名患者(11%)出现急性肾衰竭,低正常Pao2组有6名患者(2.9%)和高正常Pao2组有7名患者(3.6%)出现急性心肌梗塞。
按治疗组划分的SOFARANK结果累积值
综上,在多器官功能衰竭危重病人中,与高Pao2正常值目标相比,低Pao2正常值目标的治疗并没有导致器官功能障碍的统计学上的明显减少。
参考文献:
Effect of Low-Normal vs High-Normal Oxygenation Targets on Organ Dysfunction in Critically Ill Patients: A Randomized Clinical Trial. JAMA. Published online August 31, 2021. doi:10.1001/jama.2021.13011
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





















#危重病#
96
#功能障碍#
78
#危重病人#
91
#浓度#
68
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
79