一波三折!患者PCI术后40天再现心包压塞
2018-05-25 韩雅玲 王祖禄 朱鲜阳 规避陷阱:心血管疾病介入并发症防治攻略
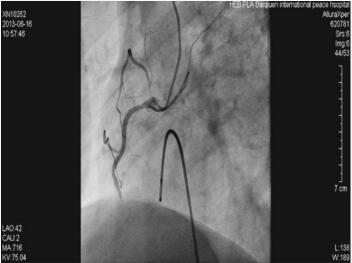
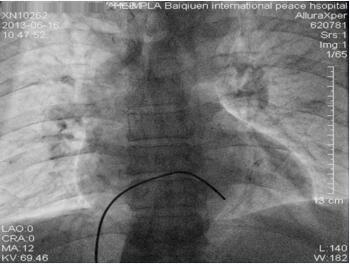
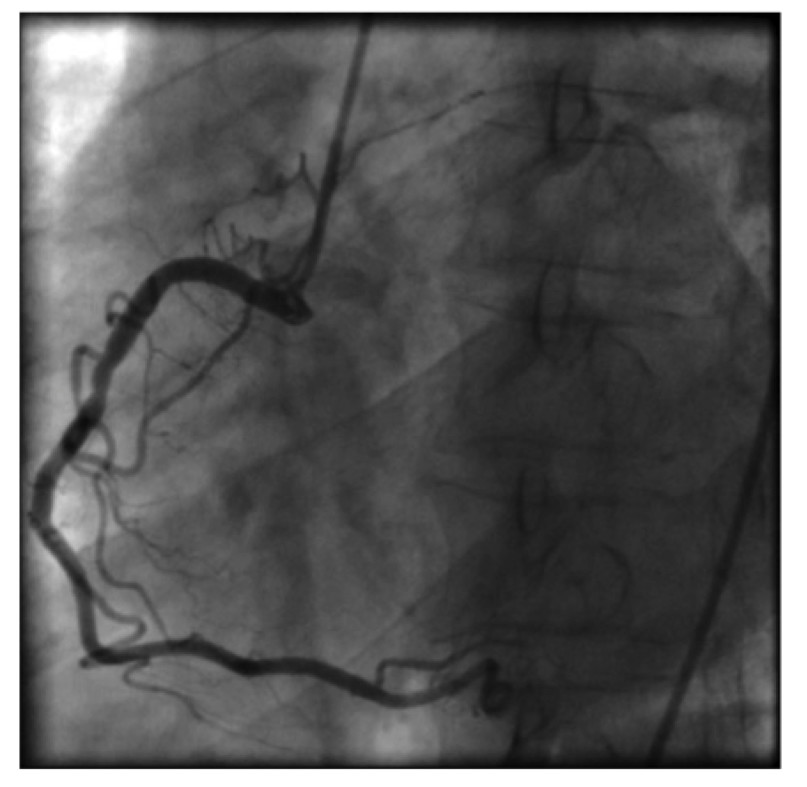
67岁男性患者因“胸闷5小时”入院,给予常规治疗未见好转,遂行冠状动脉造影及支架手术。术后患者胸闷症状缓解,然而,术后反复出现起搏功能不良,超声提示大量心包积液,考虑临时起搏电极穿孔导致急性心包压塞,行心包引流,术后一周出院。术后40天患者再次出现心包积液。为何PCI术后会出现心包压塞?该患者再次出现的原因又是什么?详见以下病例——



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PCI术#
69
好文献学习了
98
#PCI术后#
78
好文献学习了
94
典型病例分析.学习了.
98