Chest:实体瘤和脓毒症休克患者28天死亡率的结局和预测因素
2022-06-14 MedSci原创 MedSci原创
实体瘤和感染性休克患者28天死亡率相当高。与生存恶化相关的因素包括晚期肿瘤疾病、较差的工作状态、高乳酸血症和伴随的急性呼吸衰竭。应考虑对虚弱的感染性休克和晚期转移性疾病患者进行早期治疗目标讨论。
癌症是世界上第二大常见死因。然而,癌症早期诊断和治疗的进步降低了癌症患者的总体死亡率。以美国为例,从1991年-017年,癌症的总死亡率下降了29%。这一下降主要归因于肺癌生存率的改善,肺癌生存率占所有癌症死亡的四分之一。尽管如此,越来越多的活动性癌症患者面临着发生危及生命的并发症的风险,如脓毒症和感染性休克。但是使用第三国际共识定义(Sepsis-3)评估实体肿瘤患者感染性休克结局的数据很少。
此外,重症成人实体瘤合并感染性休克28天死亡率的独立预测因素也未明确。

近日,呼吸领域权威杂志chest上发表了一篇研究文章,研究人员组建了因感染性休克而住进重症监护病房(ICU)的实体肿瘤患者队列。研究人员从电子健康记录中收集了人口学和临床特征。研究人员开发了一个简化的多变量logistic回归模型来确定28天死亡率的独立预测因素,并使用Kaplan-Meier图来评估患者生存率。
该研究共纳入了271例患者。中位年龄为62岁(范围为19-94岁);57.2%为男性,53.5%为白人。最常见的恶性肿瘤是肺癌(19.2%)、乳腺癌(7.7%)、胰腺癌(7.7%)和大肠癌(7.4%)。大多数(84.5%)患者伴有转移性疾病。188例(69.4%)患者入住ICU28天后死亡。非幸存者的晚期癌症发生率较高,ICU前住院时间较长,入院时和整个ICU期间序贯器官衰竭评估评分较高(P<0.001)。
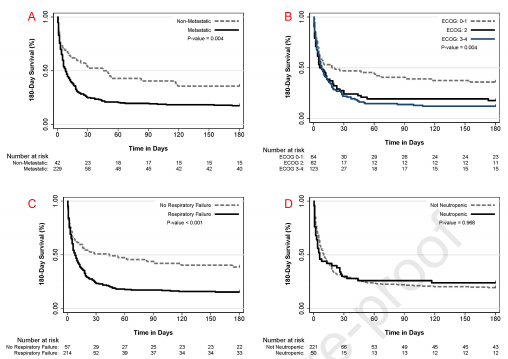
多变量分析确定了转移性疾病(比值比[OR]为3.17;95%CI为1.43-7.03)、呼吸衰竭(OR为2.34;95%CI为1.15-4.74)、乳酸水平升高(OR为3.19;95%CI为1.90-5.36)、东部合作肿瘤组表现得分为3或4分(OR为2.72;95%CI为1.33-5.57)为患者28天死亡率的独立预测因子。只有38名患者(14%)在没有医疗救助的情况下出院。
由此可见,实体瘤和感染性休克患者28天死亡率相当高。与生存恶化相关的因素包括晚期肿瘤疾病、较差的工作状态、高乳酸血症和伴随的急性呼吸衰竭。应考虑对虚弱的感染性休克和晚期转移性疾病患者进行早期治疗目标讨论。
原始出处:
John A.Cuenca.et al.Outcomes and predictors of 28-day mortality in patients with solid tumors and septic shock defined by Sepsis-3 criteria.chest.2022.https://www.sciencedirect.com/science/article/pii/S0012369222010443.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脓毒症休克#
0
#Chest#
140
#EST#
89
#预测因素#
119
学习努力
105