Cell Host Microbe:重磅!科学家首次开发出彻底治疗便秘的细菌性疗法
2018-06-23 佚名 细胞
一项刊登在国际杂志Cell Host & Microbe上的研究报告中,来自梅奥诊所的研究人员通过对小鼠进行研究发现,遗传工程化的细菌或有望作为治疗便秘的新疗法,这一研究意义非常重大,因为目前市场上几乎没有经过批准用于治疗便秘的疗法。
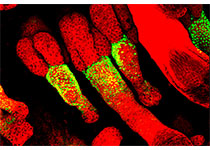
由于机体微生物组对于每个人而言都是独一无二的,而且一般的益生菌并不适合每一个人,益生菌是一种能帮助机体消化的细菌。这项研究中,研究人员开发出了遗传工程化的细菌,其能够产生大量化学色胺类物质,相比其它便秘药物而言,这些物质能帮助食物通过肠道消化,同时并不会产生太多副作用。
研究者Purna Kashyap表示,色胺类似于化学物质血清素(serotonin),血清素是在机体肠道中产生的,这项研究中我们发现色胺能够激活小鼠肠道中对血清素能够产生反应的特殊受体,从而促进结肠内壁体液的分泌;这些工程化的细菌则能够通过色胺给小鼠肠道受体施加作用来促进结肠组织分泌水分,从而加速食物穿过胃肠道组织。
很多年来,便秘的人群通常都会被医生们建议改变其饮食习惯,但通常这或许并不奏效,因为每个人机体的基因和微生物组或许都是独一无二的;研究人员所改造的工程化细菌或能通过消化系统,在不影响机体饮食和微生物群落的前提下,促进机体对食物的消化。这些细菌所产生的色胺在机体肠道内通常会快速降解,而且似乎并不会在血液中出现水平增加的情况,但却能降低胃肠道外部的副作用风险,而治疗便秘的其它药物则会影响机体的不同区域,比如心脏等。
研究者Kashyap说道,我们的研究目的就是寻找能够仅对胃肠道产生影响且并不会影响机体其它部位功能的新型疗法,除此之外,本文研究对于后期研究诸如肠易激综合征等胃肠道障碍也提供了新的思路,后期我们还需要进行额外的临床前研究来证实本文的研究结果,相关研究结果进入人类临床试验或许至少需要3年时间。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
69
#CRO#
77
#细菌性疗法#
68
#Micro#
129
#Cell#
63
#重磅#
59
学了
111
学了
110