ASH 2017:BCL2抑制剂venetoclax与伊布替尼联用治疗初诊未治高危和复发难治CLL的二期临床研究结果
2017-11-19 肿瘤资讯血液编辑 肿瘤资讯
BTK抑制剂伊布替尼(IBR)已被批准用于慢性淋巴细胞白血病(CLL)的治疗。BCL2抑制剂Venetoclax(VEN),被批准用于接受过治疗并伴17p- CLL患者的治疗。IBR与VEN联合用药的原理包括如下几个方面:1)预试验显示IBR与VEN具有协同作用;2)两药联用不导致毒性增加;3)两药具有不同的作用机制;4)两药在疾病治疗方面具有互补效应。在此对IBR与VEN联用治疗CLL的二期
研究背景:
BTK抑制剂伊布替尼(IBR)已被批准用于慢性淋巴细胞白血病(CLL)的治疗。BCL2抑制剂Venetoclax(VEN),被批准用于接受过治疗并伴17p- CLL患者的治疗。IBR与VEN联合用药的原理包括如下几个方面:1)预试验显示IBR与VEN具有协同作用;2)两药联用不导致毒性增加;3)两药具有不同的作用机制;4)两药在疾病治疗方面具有互补效应。在此对IBR与VEN联用治疗CLL的二期临床试验初步结果进行报道。
研究方法:
研究纳入两组患者,组1为复发难治CLL患者,组2为至少具有一项高危临床特征的初诊未治CLL患者,包括17p-、TP53突变、IGHV无突变状态以及年龄≥65岁。入组标准包括:年龄≥18岁,ECOG≤2分,肾功能无明显异常(肌酐清除率>50ml/min)以及肝功能正常(ALT和AST≤正常上限3倍,总胆红素≤正常上限1.5倍)。治疗起始3个月给予IBR单药420mg qd口服治疗,3个月后给予VEN治疗,每周加量直至达到目标剂量400mg qd,可以继续IBR治疗,VEN用药时间为2年。主要研究终点为获得CR/CRi。计划纳入78例患者,两组各39例。用国际慢淋工作组(IWCLL)2008标准对进行疗效评估,包括骨髓缓解情况。第1年每3个月进行一次CT检查,以后每6个月进行一次CT检查。用4色流式法(敏感性10-4)对骨髓标本进行微小残留病灶(MRD)评估。
研究结果:
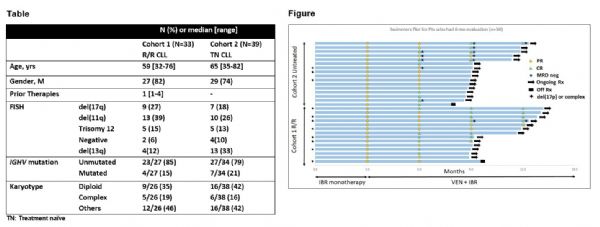
自2016年8月,72例患者接受了治疗,组1有 33例,组2有39例。中位随访时间7.5个月(范围:0.6-12.2个月)。患者基线特征见表。总计61例患者完成了IBR单药治疗并开始VEN剂量加量治疗。3个月IBR治疗后,51%(31/61)的患者发生低危TLS,2例在VEN治疗起始发生高危TLS。
组1中,29例患者接受IBR单药治疗后开始VEN剂量加量治疗。14例患者接受了至少3个月两药联合治疗,均产生疗效反应,9例患者获得CR/CRi,5例患者获得PR。加入VEN使得骨髓受累显着降低(见图),几例细胞遗传学高危患者治疗后MRD<0.1%甚至MRD转阴。
组2中,32例接受IBR单药治疗后开始VEN剂量加量治疗。16例患者接受了至少3个月两药联合治疗,均产生疗效反应,9例患者获得CR/CRi,7例患者获得PR。加入VEN后部分患者骨髓MRD阴性(见图)。
总体上来说,24%的患者需要IBR剂量减量,18%的患者需要VEN剂量减量。最常见的剂量减量原因为中性粒细胞减少。8例(11%)患者发生心房颤动,可能是IBR的不良反应。1例患者发生实验室TLS,无患者发生临床TLS。10例患者中途退组,组1、组2各5例;其中6例在IBR单药治疗中分别由于皮疹(2例)、高血压(1例)、步态不稳(1例)、需要长时间唑类治疗(1例)、感染(1例)以及撤回知情同意(1例)退组;4例患者在开始VEN治疗后分别由于血细胞减少(1例)、霍奇金转化(1例)、高血压(1例)以及第二肿瘤(输卵管癌,1例)退组。
结论:
IBR与VEN联合用药治疗CLL是安全而有效的,其有效性的初步结果令人鼓舞。联合用药3个月部分患者获得骨髓MRD转阴,表明联合用药可以对骨髓受累疗效显着。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#二期临床#
82
#2抑制剂#
104
#研究结果#
67
#抑制剂#
58
#复发难治#
83
#NET#
77
#联用治疗#
62
#伊布替尼#
49
#ASH#
57
#BCL2#
75