Cancer Cell:揭示白血病干细胞存活机制有助药物开发
2012-02-15 towersimper 生物谷
一项新研究瞄准顽固的被认为造成癌症抵抗治疗和复发的癌干细胞(cancer stem cell, 译者注:也常译作癌症干细胞或肿瘤干细胞)。这项研究于2012年2月14日发表在《细胞》子刊《癌细胞》期刊上,为揭示与白血病干细胞存活相关联的机制提供启示,同时鉴定出一个这些危险性地持续存在的细胞的特异性潜在治疗靶标。 慢性髓细胞白血病(chronic myelogenous leukemia, CML
一项新研究瞄准顽固的被认为造成癌症抵抗治疗和复发的癌干细胞(cancer stem cell, 译者注:也常译作癌症干细胞或肿瘤干细胞)。这项研究于2012年2月14日发表在《细胞》子刊《癌细胞》期刊上,为揭示与白血病干细胞存活相关联的机制提供启示,同时鉴定出一个这些危险性地持续存在的细胞的特异性潜在治疗靶标。
慢性髓细胞白血病(chronic myelogenous leukemia, CML)是一种白细胞癌症,当前人们对抗这种疾病的一线治疗方法就是使用酪氨酸激酶抑制剂。这些药物延长存活时间,但是当药物治疗停止之后,人们经常观察到病人癌症复发。美国加州杜瓦迪市希望之城国家医学中心Ravi Bhatia博士也是这篇研究的共同通讯作者。他解释道,“酪氨酸激酶抑制剂不会消灭掉白血病干细胞,这就保留着造成癌症复发的一种潜在性来源。CML病人需要无限期地服用酪氨酸激酶抑制剂,而这又会伴随着极大的毒性风险,依从性缺乏,耐药性,癌症复发和相关联的用药费用。”
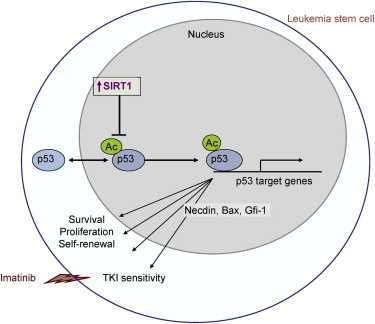
因此要成功治疗这种疾病,制定出靶向白血病干细胞的策略是必需的。以前的研究暗示酶sirtuin 1 (SIRT1)在保护干细胞免受胁迫过程中发挥着作用而且它也在白血病和其他类型癌症中起着作用。在当前的研究中,Bhatia博士、共同作者 WenYong Chen博士、第一这作者Ling Li和他们的同事们研究了SIRT1是否参与慢性髓细胞白血病干细胞存活和生长。研究人员发现SIRT1在慢性髓细胞白血病干细胞中过量表达,而且抑制 SIRT1选择性地降低慢性髓细胞白血病干细胞的存活和生长。重要的是,抑制SIRT1与p53肿瘤抑制物的激活相关联。
综上所述,这些结果揭示一种支持白血病干细胞存活的特异性机制。Chen博士作出结论,“我们的研究发现是非常重要的,因为它们证实SIRT1介导的p53失活促进慢性髓细胞白血病干细胞存活和抵抗酪氨酸激酶抑制物治疗。我们的研究结果提示着抑制SIRT1是一种选择性靶向白血病干细胞的一种有吸引力的方法,因为当前的治疗方法不能消除白血病干细胞。”
doi:10.1016/j.ccr.2011.12.020
Activation of p53 by SIRT1 Inhibition Enhances Elimination of CML Leukemia Stem Cells in Combination with Imatinib
Ling Li, Lisheng Wang, Liang Li, Zhiqiang Wang, Yinwei Ho, Tinisha McDonald, Tessa L. Holyoake, WenYong Chen, Ravi Bhatia
BCR-ABL tyrosine kinase inhibitors (TKI) fail to eliminate quiescent leukemia stem cells (LSC) in chronic myelogenous leukemia (CML). Thus, strategies targeting LSC are required to achieve cure. We show that the NAD+-dependent deacetylase SIRT1 is overexpressed in human CML LSC. Pharmacological inhibition of SIRT1 or SIRT1 knockdown increased apoptosis in LSC of chronic phase and blast crisis CML and reduced their growth in vitro and in vivo. SIRT1 effects were enhanced in combination with the BCR-ABL TKI imatinib. SIRT1 inhibition increased p53 acetylation and transcriptional activity in CML progenitors, and the inhibitory effects of SIRT1 targeting on CML cells depended on p53 expression and acetylation. Activation of p53 via SIRT1 inhibition represents a potential approach to target CML LSC.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










Cheers pal. I do apctpeiare the writing.
111
#Cell#
67
#CEL#
63
#cancer cell#
70
#白血病干细胞#
74
#药物开发#
62