Cell stem Cell:华人学者带来“吃不胖”的基因疗法,有望治疗糖尿病
2017-08-04 佚名 学术经纬
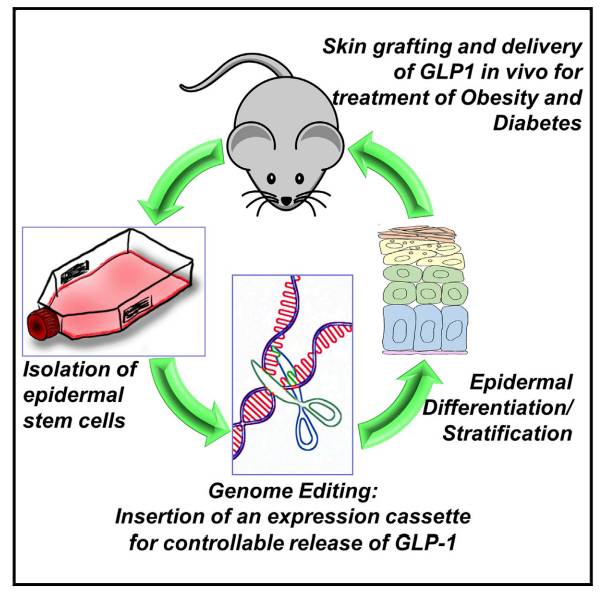
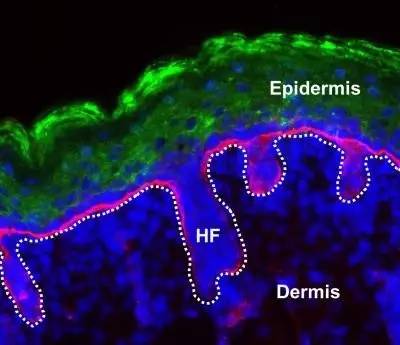
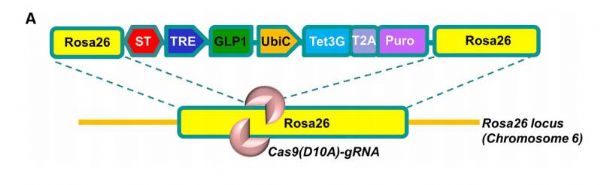
近日,在顶尖学术刊物《细胞》的子刊《Cell Stem Cell》中,来自芝加哥大学的Xiaoyang Wu教授团队发表了他们的一项新发现——将干细胞技术、CRISPR基因编辑技术、与皮肤移植技术相结合,一款基因疗法有望对肥胖症与2型糖尿病这两种常见疾病进行治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
52
#Cell#
60
#stem cell#
70
#STEM#
68
#华人#
59
#华人学者#
79
近日,在顶尖学术刊物《细胞》的子刊《Cell Stem Cell》中,来自芝加哥大学的Xiaoyang Wu教授团队发表了他们的一项新发现——将干细胞技术、CRISPR基因编辑技术、与皮肤移植技术相结合,一款基因疗法有望对肥胖症与2型糖尿病这两种常见疾病进行治疗。
90
谢谢分享,学习了
99