BMJ:荟萃分析揭示水果和蔬菜摄入量与死亡率之间的联系
2014-07-31 MedSci MedSci原创
作为健康饮食的一个关键组成部分,医生们常建议人们多食用水果和蔬菜,以来预防慢性疾病。心血管疾病和癌症是全世界死亡的两个主要原因,研究者们不断研究风险因素,减少这些重要疾病的发生,改善健康和长寿。 近年来,虽然已经有越来越多的证据表明,食用水果和蔬菜与死亡率相关,包括心血管疾病和癌症的死亡率,却依然存在争议。一些研究发现,食用水果和蔬菜能降低死亡率的风险,然而研究者观察英国素食者和非素食者
作为健康饮食的一个关键组成部分,医生们常建议人们多食用水果和蔬菜,以来预防慢性疾病。心血管疾病和癌症是全世界死亡的两个主要原因,研究者们不断研究风险因素,减少这些重要疾病的发生,改善健康和长寿。
近年来,虽然已经有越来越多的证据表明,食用水果和蔬菜与死亡率相关,包括心血管疾病和癌症的死亡率,却依然存在争议。一些研究发现,食用水果和蔬菜能降低死亡率的风险,然而研究者观察英国素食者和非素食者之间死亡率没有显著差异(Am J Clin Nutr2003;78:533S-8S)。
了解食用水果和蔬菜和死亡率之间的关系是为了引导消费者的选择和优先考虑膳食指南以降低风险。为此,山东大学公卫学院和华中科技大学同济医学院的研究人员,探究了水果和蔬菜摄入量对死亡率、心血管死亡率和癌症死亡率的影响,并首次从剂量-效应的角度进行分析。这项基于前瞻性队列研究的荟萃分析,从全新的角度分析了水果、蔬菜摄入量与人类死亡风险之间的联系。

本研究采用的计量单位为“份”,一份蔬菜的重量定义为77 g,一份水果的重量定义为80 g。 采用STATA 12.0版本(StataCorp LP)来分析数据。
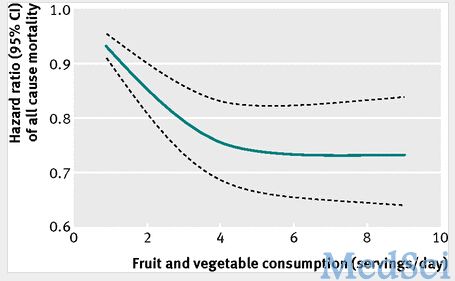
增加蔬菜和水果的摄入,能显著降低全因死亡率,尤其是心血管死亡率。若每日增加一份蔬菜/水果的摄入,则全因死亡率平均下降5%(一份蔬菜为5%。一份水果味6%)。摄入5份或更多水果/蔬菜死亡风险降低26%,但增加摄入量没有进一步降低死亡风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#摄入量#
76
#荟萃分析#
66
#荟萃#
70
#BMJ#
96
科学依据,随访时间长。
205
意料之中呀
157