COPD增加了对睡眠障碍的易感性,这可能反过来导致呼吸道症状加重。近日,呼吸领域权威杂志chest上发表了一篇研究文章,该研究在基于人群的样本中旨在评估主观睡眠质量与COPD恶化风险之间的关系。
该研究的数据来自阻塞性肺病(CanCOLD)加拿大队列研究,纳入的COPD参与者已经完成了18个月的随访。研究人员使用匹兹堡睡眠质量指数(PSQI)及其因子3得分衡量睡眠质量。以症状为基础(呼吸困难或痰液变化>48小时)和基于事件(症状加药物治疗或计划外的健康服务)的恶化进行了评估。研究人员使用负二项式回归评估了PSQI与恶化率之间的关联。研究人员同时评估了受试者无恶化存活率。
研究人员分析了480名COPD患者,其中185例在随访期间出现超过1次恶化,203例患者基线睡眠质量较差(PSQI>5)。随后基于症状恶化的参与者的中位基线PSQI评分高于没有恶化的参与者(6.0,IQR为3.0-8.0, vs. 5.0,IQR为2.0-7.0,p=0.01),并且在基线PSQI>5的受试者中更有可能(50.3% vs. 37.3%,p=0.01)。较高的PSQI评分与基于症状的恶化风险(调整后的RR为1.09,95%CI为1.01-1.18,p=0.02)和基于事件的恶化风险(调整后的RR为1.10,95%CI为1.00-1.21,p=0.048)增加相关。这种关联主要发生在未确诊的COPD患者中。最强的关联是因子3(睡眠障碍和白天功能障碍)。睡眠质量较差的参与者出现基于症状的恶化时间较短(调整后的HR为1.49,95%CI为1.09-2.03)。
由此可见,更高的基线PSQI评分与COPD恶化的风险增加相关。
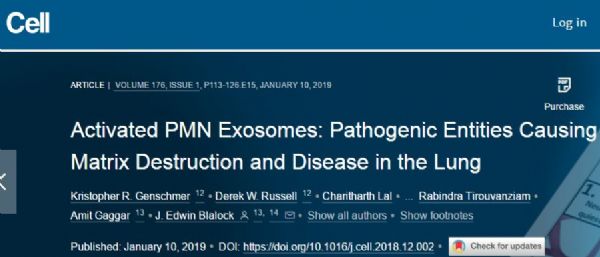
原始出处:
Matthew Shorofsky,et al.Impaired Sleep Quality in COPD is Associated with Exacerbations: The CanCOLD cohort study.chest.2019.https://doi.org/10.1016/j.chest.2019.04.132
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Chest#
70
#急性加重#
86
#EST#
78
#睡眠质量#
69
#COPD患者#
62
学习了,谢谢分享。
95