Euroanaesthesia 2015:他汀控制CABG术后死亡率作用更优
2015-06-04 大鹏 译 医学论坛网
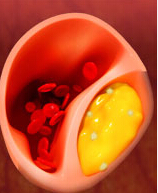
2015年欧洲麻醉会议(Euroanaesthesia)收录了一项临床试验报告,其研究结果显示,心脏冠状动脉旁路移植(CABG)术前他汀治疗可以显著降低患者死亡率,而且这种效果是其他几种常用心血管药物所不具备的。该研究发表于《欧洲麻醉学杂志》(European Journal of Anaesthesiology)。术前心血管药物治疗可以影响围手术期一系列风险指标。他汀已被证实可以降低CABG围手
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












感谢作者分享
124
#ANA#
75
#EST#
71
#ESI#
80
#术后死亡率#
76
似乎仅辛伐他汀表现出这种保护作用。另一方面,其他几种药物不能降低围手术期死亡率。这个研究存在某种潜在偏倚
130