Lancet Respir Med:免疫疗法,第三波肺癌治疗新潮流—呼吸病学2015年度总结专题
2015-12-03 MedSci MedSci原创
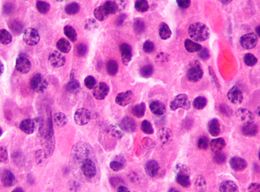
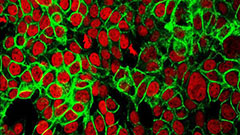
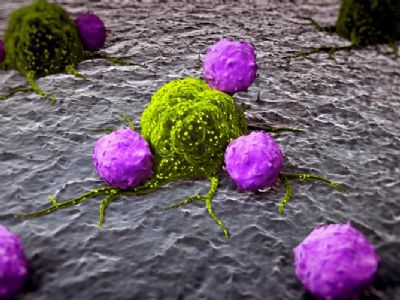
继1980年代化疗和2000年代的靶向治疗之后,免疫肿瘤学是改善非小细胞肺癌治疗效果的第三波潮流。免疫疗法对于肺癌患者有可能产生持久的治疗反应,这将是改善肺癌治疗效果的最大的潮流。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#呼吸病#
68
#Lancet#
67
#肺癌治疗#
73
#专题#
83
#呼吸病学#
71
好文章,值得收藏
197
好文章,值得收藏
143
#Med#
72