肿瘤免疫疗法——多突变癌症克星
2015-06-30 谢梦莹 译 环球科学
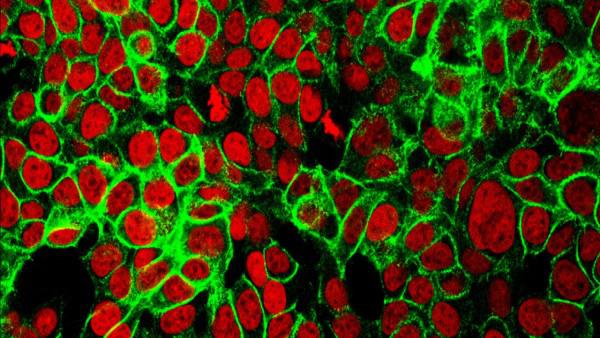
肿瘤中的基因突变越多,新免疫疗法就越有效。人类结肠癌细胞。图片来源:URBAIN WEYEMI, CHRISTOPHE E. REDON, WILLIAM M. BONNER 临床试验中使用的新型免疫系统激活抗癌药物让许多看似无法治愈的黑素瘤或肺癌患者重获新生,但这些药物对结肠癌似乎无效。不过有一个例外——一位男性患者的结肠癌转移瘤在2007年接受药物治疗后消失了——引起了研究人员的兴趣
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












加油
41
期待有更多研究
176
现在很热,都用起来不知道是什么时候了
179
13640291462需要临床实验麻烦联系我吧
112
看看
147
#肿瘤免疫疗法#
100
PD-1最近真是大放异彩!
102