Eur Heart J:SARS-CoV-2感染后非住院个体的多器官评估
2022-01-07 MedSci原创 MedSci原创
从轻度至中度SARS-CoV-2感染中恢复的受试者表现出与肺脏、心脏、血栓形成和肾功能相关的亚临床多器官病变迹象,而没有结构性脑损伤、神经认知或生活质量受损的迹象。
SARS-CoV-2感染后可能会出现长期后遗症。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,与普通人群的对照者相比,研究人员旨在全面评估轻度至中度SARS-CoV-2感染后个体的器官特异性功能。
在首次SARS-CoV-2检测呈阳性后的中位9.6个月内,443名非住院的患者接受了检查,并根据年龄、性别和教育程度匹配了来自德国人群队列的1328名对照者。

研究人员评估了肺脏、心脏、血管、肾脏和神经系统的状态,以及与患者相关的结局。研究人员采用身体体积描记术记录了SARS-CoV-2感染后肺总量(回归系数为-3.24,调整后的P=0.014)和更高的特定气道阻力(回归系数为8.11,调整后的P=0.001)。
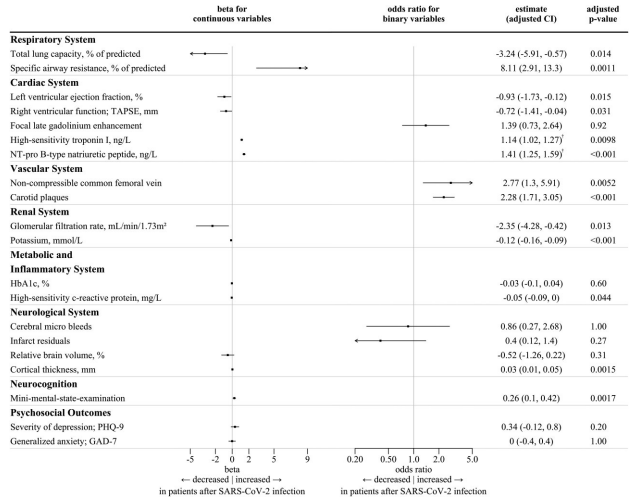
与匹配的对照组相比,SARS-CoV-2感染后患者心脏评估显示左心室(经胸超声心动图左心室射血分数回归系数为-0.93,调整后P=0.015)和右心室功能的测量值略低,心脏生物标志物浓度较高(高敏肌钙蛋白为1.14,B型利钠肽前体N末端为1.41,调整后的P≤0.01),但心脏磁共振成像结果没有显著差异。在SARS-CoV-2感染后,超声不可压缩的股静脉提示深静脉血栓形成的频率明显更高(比值比为2.68,调整后的P<0.001)。SARS-CoV-2感染后肾小球滤过率(回归系数-2.35,调整后的P=0.019)较低。相对脑容量、脑微出血的患病率和梗塞残留物两组相似,而SARS-CoV-2感染后皮质厚度更高,认知功能没有受损。同样,与两组患者结局也没有差异。
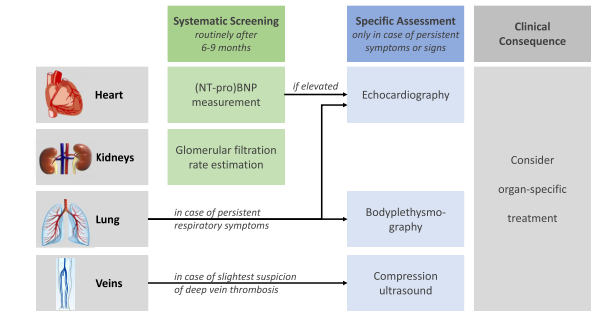
由此可见,从轻度至中度SARS-CoV-2感染中恢复的受试者表现出与肺脏、心脏、血栓形成和肾功能相关的亚临床多器官病变迹象,而没有结构性脑损伤、神经认知或生活质量受损的迹象。相应的筛查可以指导进一步的患者管理。
原始出处:
Elina Larissa Petersen, et al.Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab914/6499078
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#SARS-CoV#
71
学习学习学习
86
#SARS#
66
#ART#
69
#HEART#
59
学习学习学习
171