Lancet:放置心房分流器并不能减少心力衰竭事件发生率!
2022-02-03 Nebula MedSci原创
心房分流器的放置并没有减少心力衰竭事件的总发生率,也没有改善射血分数大于或等于40%的心力衰竭患者的健康状况
运动时,左心房压力负荷增加引发呼吸困难是射血分数保留或轻度降低的心力衰竭的标志。放置心房分流器可降低此类心衰患者运动时的肺毛细血管楔压。
该研究目的是评估心房内分流术是否可以减少这类患者的心衰事件或改善其健康状况。
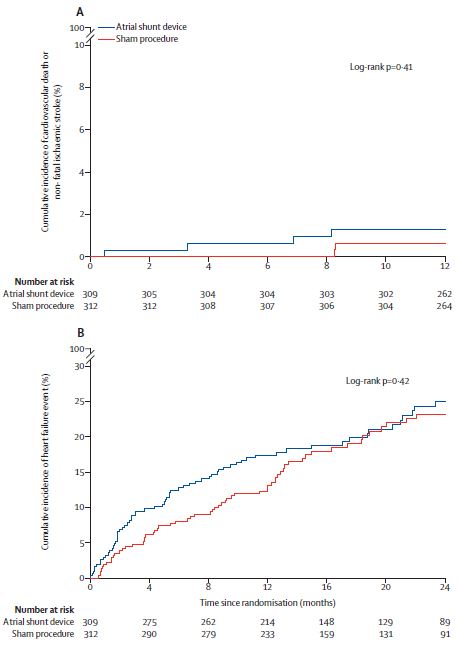
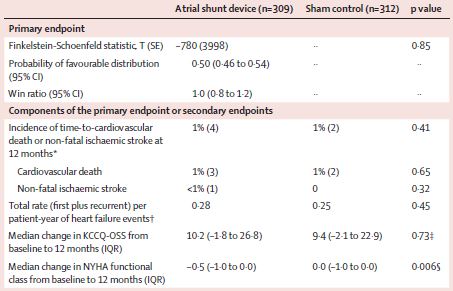
这是一项随机、国际化、双盲、假-对照的临床使用,招募了年满40岁的有症状的心脏射血分数≥40%的心衰患者。随机1:1分成两组,接受放置心房分流器或假手术。主要终点是12个月时心血管死亡或非致死性缺血性卒中的分层复合、24个月内的总心衰发生率和12个月时堪萨斯城心肌病问卷总结评分的变化
主要疗效终点
2017年5月25日至2020年7月24日,共招募了1072位患者,其中626位被随机分到了心房分流器组(n=314)或假手术组(n=312)。两组的主要复合终点无明显差异(p=0.85),每个单终点也无组间差异。预定的亚组分析显示,心房分流器治疗对性别、右心房体积指数和运动20W水平时肺动脉收缩压不同的亚组有不同的治疗效果(男性、右心房体积指数≥29.7mL/m2和肺动脉收缩压>70mmHg的个体的预后均更差)。此外,两组间的复合安全性终点无明显差异。
详细的疗效终点
总之,心房分流器的放置并没有减少心力衰竭事件的总发生率,也没有改善射血分数大于或等于40%的心力衰竭患者的健康状况。
原始出处:
Sanjiv J Shah, et al. Atrial shunt device for heart failure with preserved and mildly reduced ejection fraction (REDUCE LAP-HF II): a randomised, multicentre, blinded, sham-controlled trial. The Lancet. February 01, 2022. https://doi.org/10.1016/S0140-6736(22)00016-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生率#
87
#Lancet#
90
#心房#
84
建议批准该口服抗病毒药物用于治疗不需
0
讲得太好了,很喜欢这个软件
106