语言是人类先进而重要的功能,语言障碍可能发生在许多脑部疾病的情况下,包括中风、肿瘤、创伤等。但语言功能障碍是可变的,当颅内原发疾病稳定或消除后,患者可能在一定程度上恢复其语言功能。这种现象被认为是归因于语言重组,这一点已被广泛研究。然而,上述疾病几乎都是后天性的,而且通常是在语言学习期过后很久才发生。因此,这些疾病为已建立的语言网络受损后的功能重组提供了一个模型。
相反,涉及语言区域的先天性病变可以从另一个角度提供一个语言重组的研究模型。脑动静脉畸形(AVM)被认为是一个理想的例子。脑动静脉畸形被认为是一种先天性病变,其病灶由各种异常血管组成,动脉和静脉之间直接相连。
它发生在语言学习和建立语言网络的时期之前。然而,涉及传统语言区的未破裂的AVM患者在其一生中通常不会出现语言障碍。这种独特的模式是,当传统语言功能区在语言习得期之前受损时,其他脑区可能在语言学习期参与到语言网络中,以弥补随后的功能损失。
然而,关于脑AVMs语言功能可塑性的研究是有限的,具体的皮质和皮质下损伤和重塑机制仍不清楚,特别是AVMs不同位置的语言相关白质(WM)变化,可能反映了不同的皮质下语言重组机制。
此外,语言网络很复杂,有许多纤维束参与。根据语言处理的双流模型,语言网络由两条不同的通路组成:背侧和腹侧通路。背侧通路的主要纤维束是上纵束(SLF)和弓状束(AF)。而腹侧通路主要包括下额枕部筋膜(IFOF)、下纵筋膜(ILF)、钩状筋膜(UF)和丘脑前辐射(ATR)。所有这些纤维束都参与了语言处理并发挥了不同的作用。
同时,扩散张量成像(DTI)是一种非侵入性的磁共振成像技术,可以测量脑组织中的水扩散各向异性。可以从DTI数据集中提取的定量指标,如各向异性(FA)、轴向扩散率(AD)、径向扩散率(RD)和平均扩散率(MD),通常对检测中枢神经系统中轴突和髓鞘的微观异常很敏感。
此外,分析和建模方法,如自动纤维定量(AFQ)已经被开发出来,以更好地描述WM的完整性和神经束的方向。作为一种完全自动化的方法,主要的WM纤维束可以通过AFQ可靠地识别出来,这有利于进一步对解剖学上同等位置的纤维束进行定量和统计分析,这已被应用于衰老和精神分裂症的研究中,但尚未应用于AVM研究。对有语言障碍的AVM患者的全脑主要纤维进行完整的可视化和量化,可能会揭示自出生以来疾病发展过程中语言处理的障碍和可塑性机制。
藉此,天坛医院的Xiaofeng Deng等人,招募了涉及不同语言区域的AVM患者,并进行了这项研究,利用AFQ方法从结构连接的角度来证明语言重组的机制。

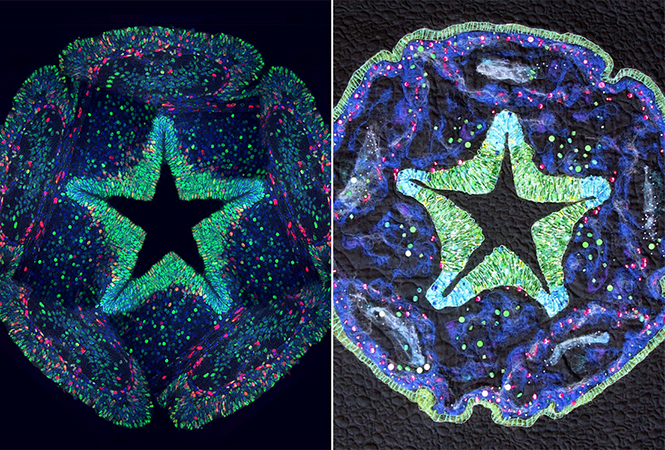
他们前瞻性地招募了33名涉及语言区的AVMs患者。根据病变位置将患者分为3组:额叶组(14名患者)、颞叶组(15名患者)和顶叶组(4名患者)。30名年龄和性别相匹配的健康对照组作为对比入选。所有参与者都进行了弥散张量成像扫描,并应用自动纤维量化方法定量研究3个AVM组与对照组之间的语言相关白质连接的差异。
根据Western Aphasia Battery测试,所有受试者的语言功能均正常。在额叶组,各向异性(FA)值在left arcuate fascicle中下降,在left superior longitudinal fasciculus and uncinate fascicle上升;
在颞叶组,FA值在 left inferior fronto-occipital fascicle and inferior longitudinal fascicle 下降,在right anterior thalamic radiation and uncinate fascicle上升。

在顶叶组,left arcuate fascicle and inferior longitudinal fascicle的FA值下降,双侧bilateral anterior thalamic radiations and uncinate
fascicles and right inferior fronto-occipital fascicle的FA值上升。
在FA值下降的纤维束中,径向扩散性的增加很常见,而FA值增加的纤维束通常伴随着轴向扩散性的增加。
该研究的重要意义在于发现了:当传统语言区被AVM结节累及时,语言相关白质会发生重塑,其重组模式随AVM结节的位置不同而不同。级联损伤主要由髓鞘缺失引起,其可塑性可能由轴突重塑过程主导。
原文出处:
Deng X, Yin H, Zhang Y, et al. Impairment and Plasticity of Language-Related White Matter in Patients With Brain Arteriovenous Malformations. Stroke. Published online December 2021:STROKEAHA.121.035506. doi:10.1161/STROKEAHA.121.035506
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#静脉#
82
#动静脉畸形#
0
#白质#
85
#畸形#
90
#损伤#
68
#语言#
79