Neurology:多发性硬化患者,抑郁或增加血管疾病和死亡风险
2021-09-06 Freeman MedSci原创
抑郁症与多发性硬化症患者,发生血管疾病和死亡的风险增加有关,抑郁症和多发性硬化症对全因死亡的影响是协同的。
以前的研究表明,抑郁症是多发性硬化症(MS)患者最常见的合并症,在任何特定的时间点上影响着21-24%的MS患者。这明显高于普通人群,并与多种不良后果相关,包括残疾进展和健康相关的生活质量下降。
在普通人群中,抑郁症与患血管疾病的相对风险增加(30%)和全因死亡的相对风险增加(70%)有关。
此外,抑郁症越严重,血管疾病的发病风险和相关死亡率就越高。然而,在多发性硬化症人群中,对这些关联的了解要少得多。
丹麦的一项研究发现,精神病合并症,包括双相情感障碍和精神病,与全因死亡率的增加有关,但没有包括一个对照组,因此不能确定这种关联的程度是否与一般人群不同。
加拿大的一项研究报告表明,多发性硬化症和抑郁症对所有病因死亡率的影响大于相加的作用。多发性硬化症、精神病合并症和血管风险之间的关联可能也存在性别差异。女性多发性硬化症患者的心血管疾病发病率较低,但抑郁症的发病率较高,心血管疾病的死亡风险也高。
藉此,帝国理工学院的Raffaele Palladino等人,评估多发性硬化症患者与年龄、性别和普通医生匹配的对照组相比,抑郁症、血管疾病和死亡率之间的关联是否有所不同。还评估多发性硬化症和抑郁症对血管疾病风险和死亡率的影响是否大于相加效应,并探讨这些关联中可能存在的性别差异。
他们在1987年1月1日至2018年9月30日期间进行了一项基于人口的回顾性匹配队列研究,其中包括英格兰的多发性硬化症患者和没有多发性硬化症的匹配对照,按抑郁症状态进行分层。并使用时变(time-varying)的Cox比例危险回归模型来检验MS、抑郁症与发生血管疾病和死亡的时间之间的关联。分析按性别进行了分层。
12,251名多发性硬化症患者和72,572名匹配的对照者被确认。在基线时,21%的多发性硬化症患者和9%的对照组有抑郁症。与没有抑郁症的匹配对照组相比,多发性硬化症患者发生血管疾病的风险增加,无论他们是否合并有抑郁症。
患有抑郁症的对照组( controls with depression)10年全因死亡的危险是1.75倍(95%CI 1.59-1.91),没有抑郁症的多发性硬化症( MS without depression )患者是3.88倍(95%CI 3.66-4.10),而多发性硬化症和抑郁症患者是5.43倍(95%CI 4.88-5.96)。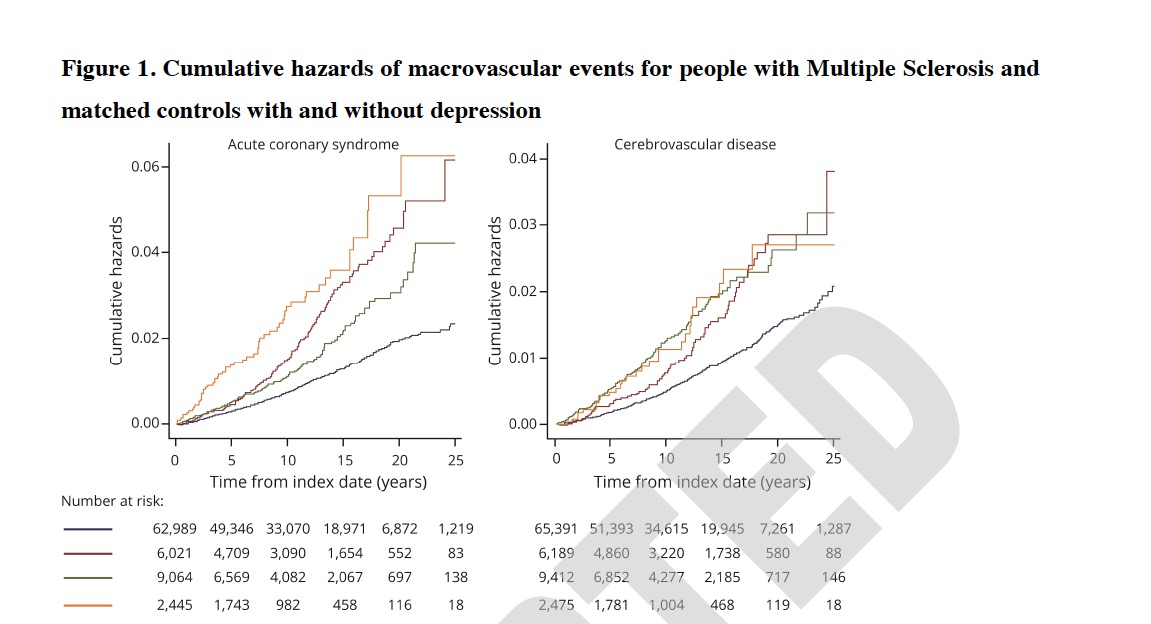
总的来说,多发性硬化症状态和抑郁症之间的相互作用是协同的,有14%的观察效果可归因于这种相互作用。
这个研究的重要意义在于发现了:抑郁症与多发性硬化症患者,发生血管疾病和死亡的风险增加有关,抑郁症和多发性硬化症对全因死亡的影响是协同的。建议进一步的研究,应评估有效治疗抑郁症是否与血管疾病和死亡风险的降低有关。
原文出处:
Palladino R, Chataway J, Majeed A, Marrie RA. Interface of Multiple Sclerosis, Depression, Vascular Disease, and Mortality: A Population-Based Matched Cohort Study. Neurology. Published online September 1, 2021:10.1212/WNL.0000000000012610. doi:10.1212/WNL.0000000000012610
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#多发性#
91
#Neurol#
60
#死亡风险#
81
#血管疾病#
71
学习
111
学到了很多东西,谢谢老师的指导
82