Thorax:婴儿期eNO水平与细支气管炎和喘息相关
2021-12-20 小文子 MedSci原创
与出生后12个月内发生细支气管炎和呼吸道症状的儿童相比,未出现该症状的婴儿6周龄时eNO水平明显较高。
呼出气中的一氧化氮(eNO)是2型免疫应答诱导的气道炎症的标志物。Thorax杂志的一项研究探索了6周龄婴儿eNO水平与妊娠期哮喘妇女所生婴儿的细支气管炎发病率和呼吸道症状之间的关系,及其与尿嗜酸性粒细胞蛋白X(EPX)的相关性。
采用前瞻性随机队列研究,研究人员对妊娠期哮喘母亲所生的6周龄婴儿进行随访,并使用快速反应化学发光分析仪测量自然睡眠期间的eNO,收集至少100次呼吸。主要结局是12月龄发生细支气管炎。6周龄时收集尿液样本,采用ELISA免疫分析法分析uEPX水平,uEPX除以肌酐浓度获得标准化值(uEPX/c)。多元线性回归和泊松回归模型研究其相关性。
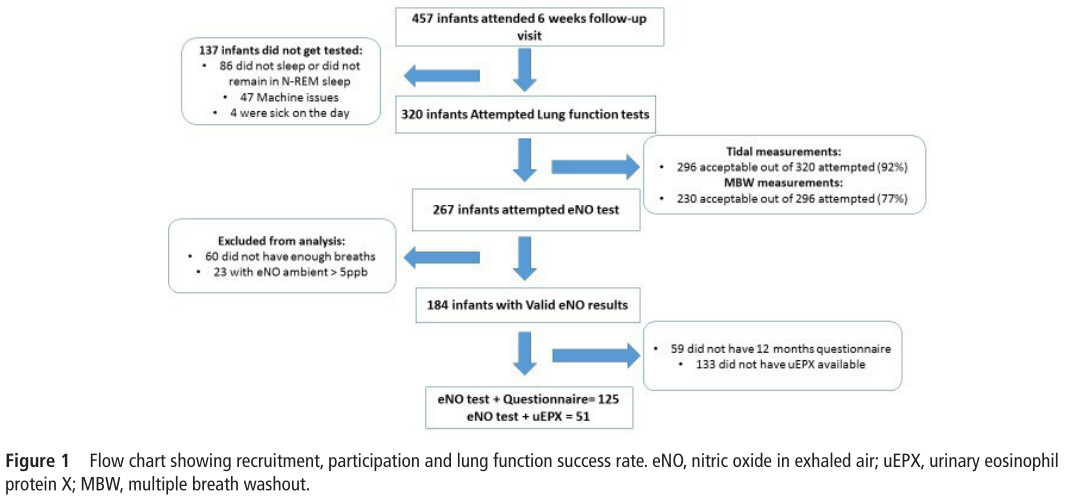
研究获得184例婴儿的eNO水平,其中125/184例(68%)获得12月龄时问卷数据,51/184例(28%)测量了uEPX/c。婴儿出生6周较高的eNO水平与较少的呼吸道症状相关(n=184,β系数:-0.49; 95%CI, -0.95 ~ -0.04,p=0.035)。eNO水平与uEPX/c呈负相关(β系数:-0.004; 95%CI, -0.008 ~ -0.001, p = 0.021)。6周龄时,有呼吸道症状和无呼吸道症状儿童的uEPX/c水平无显著差异(p=0.770)。6周龄时eNO显著较高的婴儿,出生后12个月未发生细支气管炎(p=0.038)。eNO每增加一个单位,细支气管炎、喘息、感冒或流感、短效β受体激动剂使用和复发性细支气管炎的发生风险显著降低18%~24%。
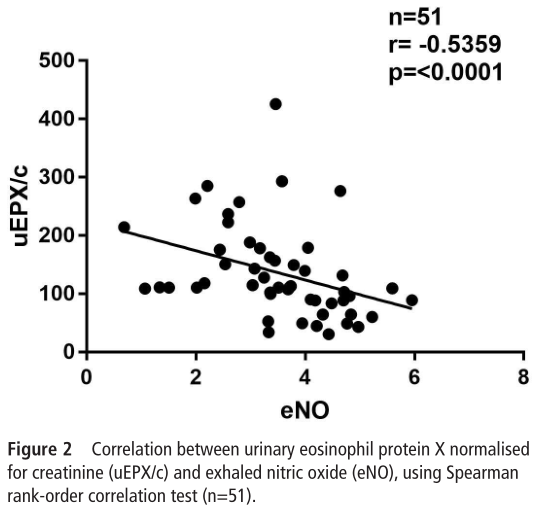
研究表明,与出生后12个月内发生细支气管炎和呼吸道症状的儿童相比,未出现该症状的婴儿6周龄时eNO水平明显较高。婴儿期eNO水平可能提示上/下气道的免疫应答改变。
原文出处:
Carla Rebeca Da Silva Sena, et al, Higher exhaled nitric oxide at 6 weeks of age is associated with less bronchiolitis and wheeze in the first 12 months of age, Thorax, 2021, doi:10.1136/thoraxjnl-2021-217299.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#细支气管炎#
113
#细支气管#
0
#支气管#
81
#婴儿期#
75