Thorac Cancer:淋巴结阳性(cN+)和阴性(cN0)的I期NSCLC患者术后无病生存(DFS)差异
2022-05-24 yd2015 网络
研究表明,在I期切除的NSCLC患者中,cN+患者的DFS较cN0患者更差。因此,对于cN+的手术切除的I期NSCLC患者,外科医生应该考虑更积极的辅助治疗或密切的随访。
识别I期非小细胞肺癌(NSCLC)患者术后肿瘤复发风险仍然是一个主要的挑战。近期,有相关结果发表在Thoracic Cancer杂志上,研究旨在比较临床淋巴结阳性(cN+)和阴性(cN0)的I期NSCLC患者术后无病生存(DFS)率。
研究纳入病理I期切除的NSCLC患者。临床N状态为1或2、病理N状态为0的患者被分为为cN+/pN0队列,而其他患者被分为为cN0/pN0队列。使用倾向评分匹配(PSM)来平衡两个队列之间的基线特征。Kaplan Meier法和Cox比例风险模型评价DFS。
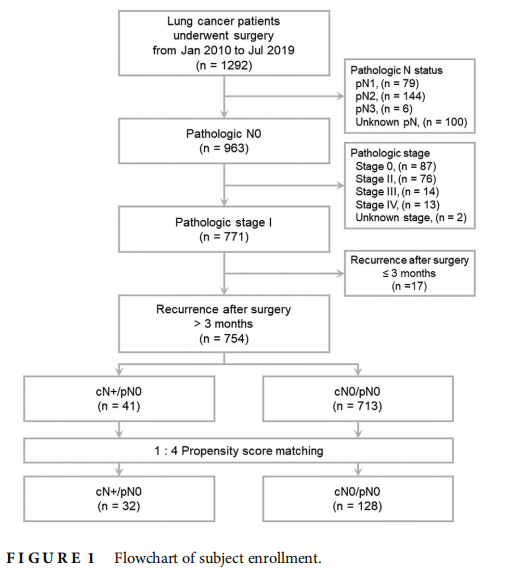
2010年1月-2019年7月,754例符合条件的患者纳入研究,其中41例(5.4%)为cN+/pN0。cN+/pN0组以CT、PET/CT、CT + PET/CT诊断临床N状态分别有8例(19.5%),8例(19.5%),和25例(61.0%)。1:4匹配后,32例患者cN+/pN0, 128例患者cN0/pN0。
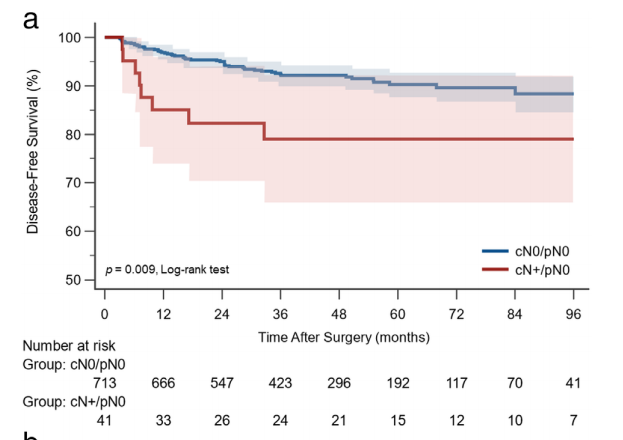
中位随访时间为43.4个月(95%置信区间[CI]: 40.9 45.6个月)。生存曲线显示,PSM前,cN+/pN0组和cN0/pN0组的5年DFS分别为79.0和90.3%。cN+/pN0患者术后复发风险高于cN0/pN0患者(p = 0.009)。PSM后,cN+/pN0和cN0/pN0组的5年DFS率分别为80.5和91.6%。匹配后的DFS仍有显著差异(p = 0.012)。
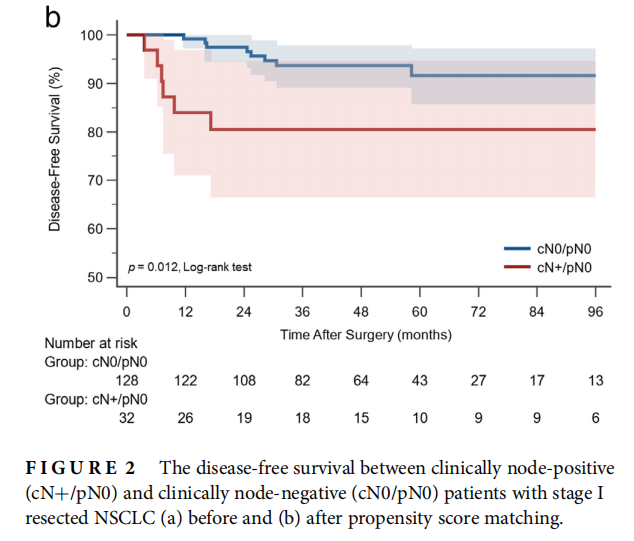
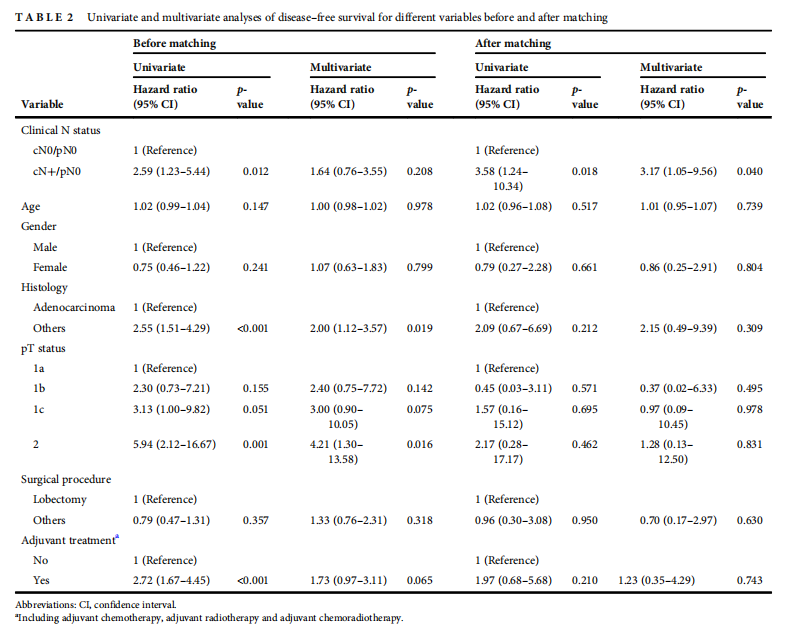
PSM前的单因素分析显示临床N状态为阳性(危险比[HR], 2.59;95% CI: 1.23-5.44;p = 0.012),非腺癌组织(HR, 2.55;95% CI: 1.51 4.29;p<0.001),较多pT2期(HR, 5.94;95% CI: 2.12-16.67;p = 0.001)和辅助治疗(HR, 2.72;95% CI: 1.67-4.45;p<0.001)与术后复发风险显著增高相关。然而,PSM前的多因素分析显示,临床N状态阳性与术后复发风险较高无关(HR, 1.64;95% CI: 0.76 -3.55;p = 0.208)。PSM后,临床N状态阳性是单因素(HR, 3.58;95% CI: 1.24-10.34;p = 0.018)和多因素(HR, 3.17;95% CI: 1.05-9.56;P = 0.040)中与术后复发较高风险独立相关的唯一因素。
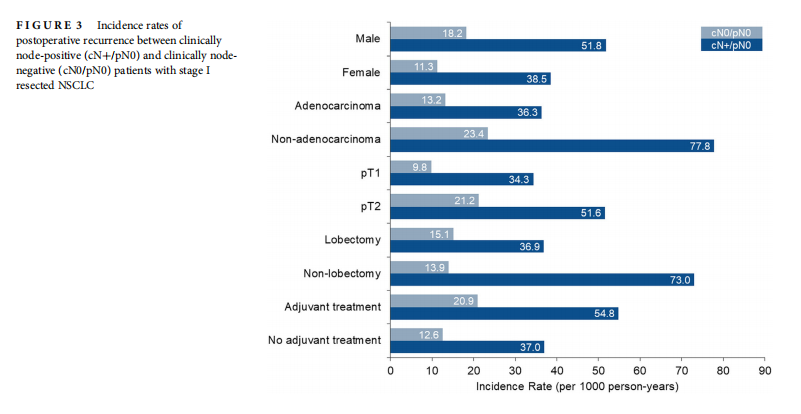
与cN0/pN0组相比,cN+/pN0组的复发率增加,而与性别、组织学、pT状态、手术程序以及有无辅助治疗无关。此外,cN+/pN0组中的非腺癌(77.8例/ 1000人年;95% CI: 9.4-281.1)和非肺叶切除术(73.0例/ 1000人年;95% CI: 8.9-263.9) 的复发率最高。
综上,研究表明,在I期切除的NSCLC患者中,cN+患者的DFS较cN0患者更差。因此,对于cN+的手术切除的I期NSCLC患者,外科医生应该考虑更积极的辅助治疗或密切的随访。
原始出处:
Huang KY, Chen HJ, Lin CH, Wang BY, Cheng CY, Lin SH. Comparison of recurrence risk between patients with clinically node-positive and -negative stage I non-small cell lung cancer following surgery: A propensity score matching analysis. Thorac Cancer. 2022 May 17. doi: 10.1111/1759-7714.14462. Epub ahead of print. PMID: 35581675.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SCLC患者#
99
#THORAC#
67
#淋巴结#
94
#NSCLC患者#
73
#淋巴结阳性#
56
坚持学习
66
值得学习
88