里程碑!全国97家医院联合发文:中药麝香保心丸联合阿司匹林使用,可使冠心病患者的心血管不良事件发生率降低26.9%
2021-04-20 MedSci原创 MedSci原创
麝香保心丸虽好,但也不能乱吃!
现在随着生活方式及饮食模式的变化,患有心血管疾病的人数越来越多。据数据显示,心血管疾病严重影响人类的健康,是成人死亡的主要原因,占全世界非传染性疾病死亡人数的45%,占所有死亡人数的31.5%。据最新的《中国心血管健康与疾病报告2019》报道,中国心血管疾病现患人数大约3.30亿,心血管疾病死亡率仍然位居首位。

pixabay
中医认为冠心病是由气虚所致心阳虚而发生的疾病,而传统中医药(TCM)有补气益血的作用可作为有益的治疗方法,并长期用于冠心病的治疗。在中国,麝香保心丸用于治疗冠心病(CAD)和心绞痛已有30余年历史,其含有多种生物活性成分,如麝香酮、人参皂苷、苏合香、蟾蜍二烯内酯、肉桂酸、沙蟾蜍精及冰片。先前多项研究已显示,麝香保心丸可扩张冠状动脉、增加冠状动脉血流量,从而缓解心绞痛症状。然而,麝香保心丸治疗冠心病仍缺乏规范合理的临床试验。
近期,由复旦大学附属中山医院葛均波院士和复旦大学附属华山医院范维琥教授领衔开展了一项符合国际规范的大型中医药循证的麝香保心丸MUST研究结果发表在Chin Med J杂志,该研究科学地评价了麝香保心丸治疗慢性稳定型冠心病患者的疗效、安全性和远期心、脑血管事件发生率,可谓中医药循证之旅的里程碑式研究。

Jun-Bo Ge , Wei-Hu Fan 2 , Jing-Min Zhou 1 , Hai-Ming Shi 2 , Fu-Sui Ji 3 , Yang Wu 4 , Yu-Lan Zhao 5 , Jun Qian 6 , Yuan-Zhe Jin 7 , Ying-Wu Liu 8 , Sheng-Huang Wang 9 , Sheng-Hu He 10 , Ping Yang 11 , Jie Wu 12 , Feng Lu 13 , Zi-Shan Hou .Efficacy and safety of Shexiang Baoxin pill (MUSKARDIA) in patients with stable coronary artery disease: a multicenter, double-blind, placebo-controlled phase IV randomized clinical trial.Chin Med J(Engl).doi: 10.1097/CM9.0000000000001257.
该研究是基于全国97家医院,共纳入2674名慢性稳定型冠心病患者,按1:1比例随机分配,接受为期24个月的麝香保心丸或安慰剂治疗。两组患者均同时按照当地三级医院操作规范接受最佳药物治疗。研究主要终点包括心血管死亡、非致死性心梗和非致死性卒中在内的主要不良心血管事件(MACE)。次要终点指标包括全因死亡、非致死性心肌梗死、非致死性卒中、因不稳定心绞痛或心力衰竭住院治疗,以及接受非计划的冠状动脉血管成形术(PCI或者CABG),心绞痛稳定性和心绞痛发作频率。
MUST研究证实,在服用阿司匹林和他汀类药物的基础上,加用麝香保心丸可降低26.9%的心血管病发生风险。长期服用麝香保心丸可以显著改善心绞痛稳定性和发作频率评分,意味着麝香保心丸可以有效缓解患者症状、显著提升患者生活质量。此外,MUST研究还证实了长期服用麝香保心丸的患者,肝肾功能及代谢相关不良事件发生率与对照组相当,体现出麝香保心丸长期应用的良好安全性。
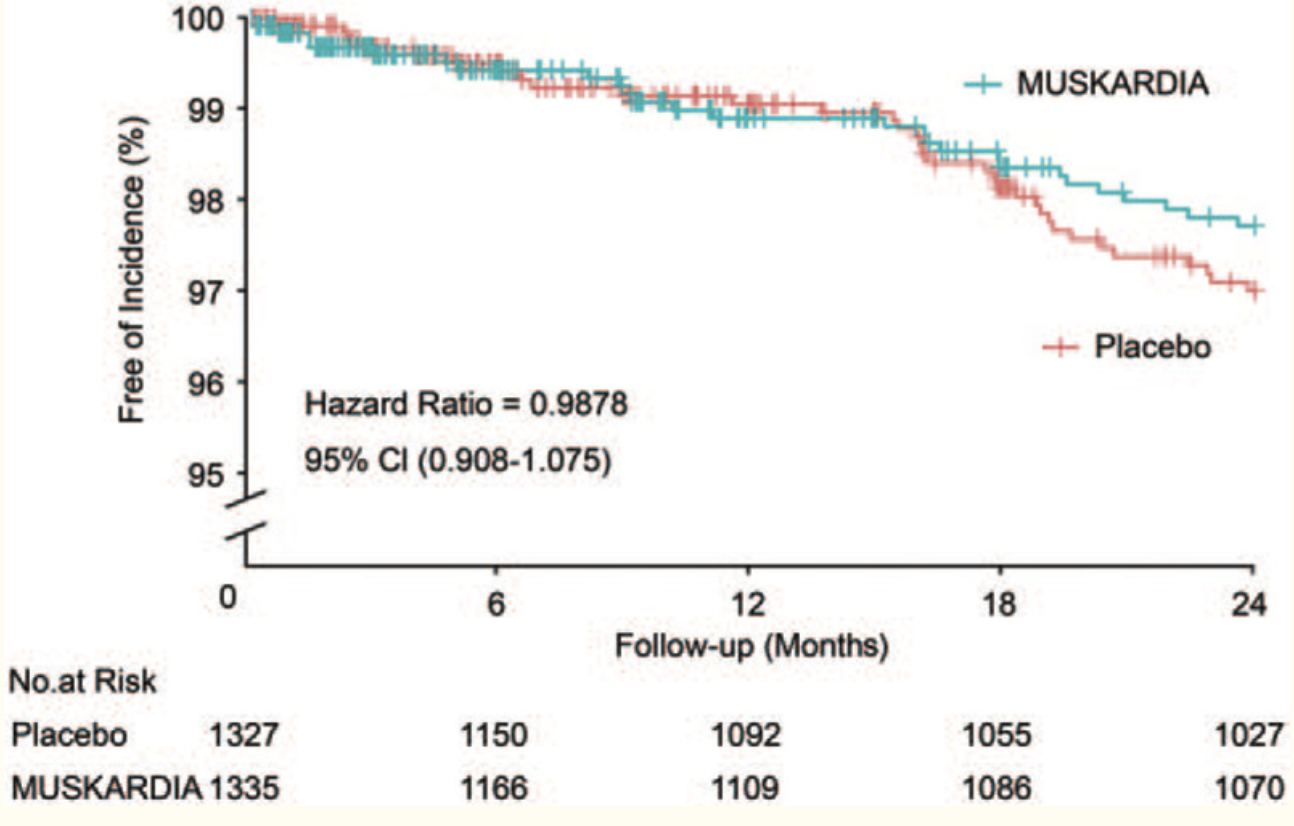
首个主要不良心血管事件发生累积时间分析.

麝香保心丸治疗18个月可改善心绞痛稳定性和频率.
具体而言,入组时,有99.7%的患者接受阿司匹林治疗,93.0%患者接受他汀类药物治疗。经过2年治疗,麝香保心丸组MACE发生率降低了26.9%。治疗18个月后,麝香保心丸组心绞痛频率显著降低。两组间其它次要终点无统计学差异,不良事件发生率也无统计学差异。

亚组分析显示麝香保心丸治疗女性和BMI <24 kg/m2的患者受益.
另外,MUST研究的亚组分析显示,麝香保心丸应用于女性和BMI <24 kg/m2的人群可显著降低MACE事件发生风险,证实麝香保心丸在女性和BMI<24 kg/m2两类人群获益更多。
自1981年麝香保心丸应用于临床以来,广泛引用于治疗冠心病,心绞痛和心肌梗死等疾病。随着现代医学的飞速发展,越来越多的科学家基于麝香保心丸的化学物质基础、药理作用及作用机制进行深入研究,并得到一定的研究结果。作为治疗冠心病心绞痛的主要药物 ,麝香保心丸通过抑制炎症反应、改善血流动力学、抑制心室重构、缩小动脉粥样硬化斑块、抗氧化损伤等多靶点多途径达到治疗效果,
虽然麝香保心丸治疗效果好,但不是想用就能用,也不是人人都适合用。2020年国家药监局发布了关于修订麝香保心丸说明书的公告,公告修订了麝香保心丸说明书上关于不良反应、禁忌和注意事项等内容。
http://www.cdr-adr.org.cn/drug_1/aqjs_1/drug_aqjs_smssggg/202011/t20201103_47976.html
不良反应监测数据显示,麝香保心丸可见以下不良反应:恶心、呕吐、腹胀、腹痛、腹泻、便秘、口干、舌下含服口腔麻木、头晕、头痛、皮疹、瘙痒、乏力、心悸、潮红等,有寒战、呼吸困难、过敏反应个案病例报告。
此外,在服用时应注意:本品建议饭后服用;脾胃虚弱者慎用;哺乳期妇女慎用;过敏体质者慎用;不宜与藜芦、五灵脂、赤石脂同用。因此,根据不同的人群和不同的情况,麝香保心丸的使用方法也不同,建议遵循医嘱。
中医药学凝聚着深邃的哲学智慧,是我国古代科学的瑰宝,也是打开中华文明宝库的钥匙,对于深化医药卫生体制改革、提高人民群众健康水平、弘扬中华文化、促进经济发展和社会和谐,都具有十分重要的意义。期待医学界能够继续以中医、西医、及中西医结合齐头并进为基础,以立足实践为根本,推动中医药循证医学发展,展望中医药现代化、国际化未来。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#里程碑#
84
#麝香保心丸#
54
#发生率#
65
赞!这波临床数据太棒了
88
#冠心病患者#
84
#心血管不良事件#
72
好
89
赞
94
学习
96
赞👍#学习#
108