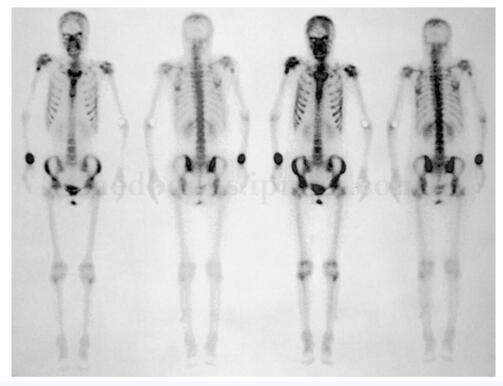
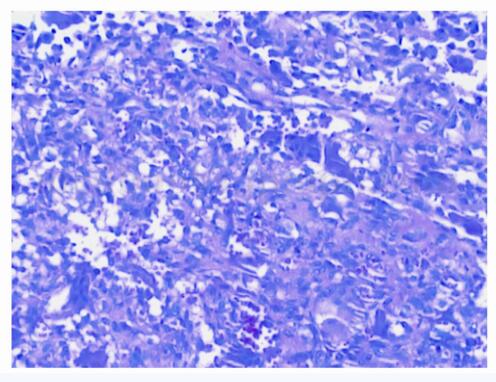
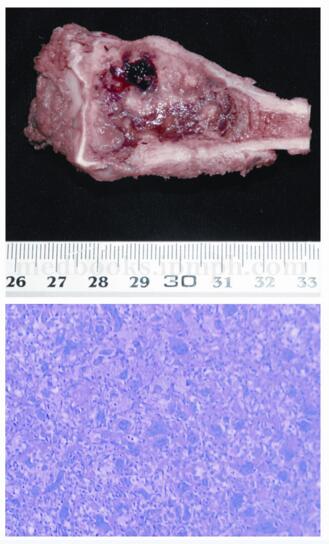
病例一则:骨巨细胞瘤放化疗均不敏感 怎么办?
2018-02-23 牛晓辉 郝林 骨肿瘤
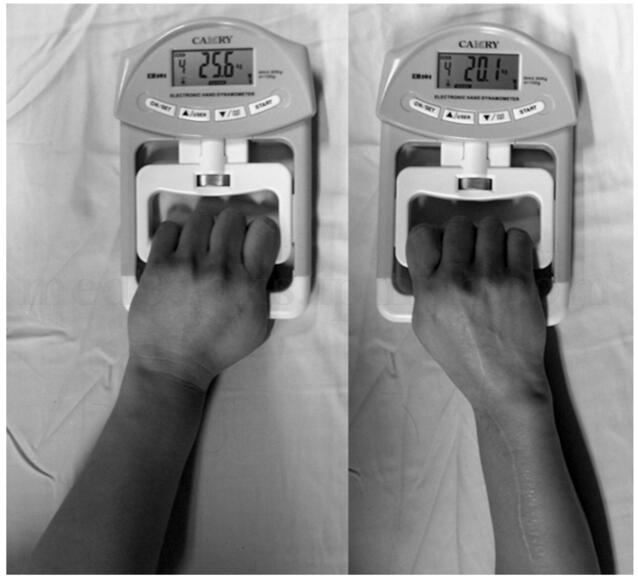
:患者,女,35岁,主因右腕关节疼痛4个月入院。患者4个月前无明显诱因出现右腕关节疼痛,活动时明显,无活动受限,无肿胀、发热,于当地医院摄片示“右桡骨远端溶骨破坏”,为求进一步诊治收入院。









本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很好的知识.学习了
101
很好的知识
101
学习了
98
#放化疗#
78
#细胞瘤#
69
#骨巨细胞瘤#
73
#巨细胞#
53
学习了.
1
一起学习学习
90
学习谢谢分享
66