Ann Rheum Dis:一种新型可靠的银屑病关节炎指炎整体超声评分(DACTOS)
2020-05-21 xiangting MedSci原创
新型DACTOS评分是一种可用于解释指炎多种超声特征的可靠指标。
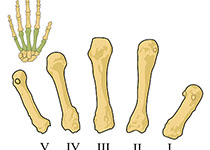
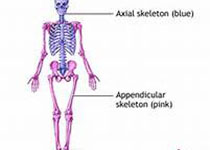
指炎是银屑病关节炎(PsA)最典型的特征之一,其终生患病率高,并被纳入PsA临床指标。肌肉骨骼超声(Msk-US)可以很容易地检测到指炎对手指解剖结构的侵袭并监测治疗效果。这项研究旨在确定PsA手部指炎的特征性病变,评估Msk-US对这些病变进行评分的可靠性,并建立一种指炎整体超声(DACTOS)评分。
在对PsA指炎使用Msk-US进行系统的文献综述后,12名风湿病专家参加了三轮Delphi程序和共识会议,以就表征指炎的超声基本病变和整体超声评分的组成达成共识。然后,进行了基于网络和基于患者的评估者内部和评估者间的可靠性练习,以评估那些纳入评分的病变。
DACTOS评分是通过将Delphi调查中选择的病变评分进行相加而获得的:皮下软组织水肿、屈肌腱鞘炎、腹膜外伸肌炎和滑膜炎。DACTOS评分的范围为0到25。在可靠性练习中,评分纳入超声病变的一致性为中等到优秀。
新型DACTOS评分是一种可用于解释指炎多种超声特征的可靠指标。DACTOS评分为手部指炎提供了有用的整体分析并有助于临床诊断,也可以作为伴指炎的PsA患者治疗和研究的有用工具。
原始出处:
Alen Zabotti. Novel and reliable DACTylitis glObal Sonographic (DACTOS) score in psoriatic arthritis. Ann Rheum Dis. May 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
70
#DACTOS#
67
#Actos#
60
#CTO#
83
#指炎#
64
#关节炎#
50