掐指一算就能预测动脉粥样硬化性心血管疾病预后?这个简易指标还真行!
2022-01-27 LILYMED MedSci原创
Sci Rep. :腰围-体质量指数比值作为动脉粥样硬化性心血管疾病患者心血管预后的人体测量预测因子
肥胖是心血管疾病,如高血压、冠状动脉疾病 (CAD)、中风和心力衰竭的独立危险因素。临床和流行病学数据表明,动脉粥样硬化性心血管疾病 (ASCVD) 的可改变危险因素(包括高血压、糖尿病和血脂异常)在超重和肥胖个体中的患病率较高。虽然BMI被广泛应用于评估肥胖,但其使用的局限性在于它无法区分脂肪量,无脂肪量和瘦体重以及皮下或内脏脂肪的分布。新出现的证据显示,在已确诊的ASCVD患者中存在一种称为"肥胖悖论"现象。其中 BMI 死亡率曲线为 U 形。也就是说,超重和轻度至中度肥胖患者反而比BMI正常和严重肥胖的患者预后更好。

众所周知,内脏脂肪组织增加与血管炎症和随后的动脉粥样硬化有关。腰围指数(如腰围(WC)和腰臀比(WHR))是中心性肥胖的两个最常见指标。这两项测量均与内脏脂肪组织相关,并与心血管事件增加相关,并且似乎比BMI更适合作为预测心血管结局的人体测量参数。然而,理论上,仅靠WC无法允许在具有不同体型和质量的个体之间进行比较。
最近,已有研究提出了两个新的基于WC的人体测量指数,即身体圆度指数(BRI)和体型指数(ABSI),一项研究表明,BRI可以识别心血管疾病和危险因素,但与BMI和WC等传统人体测量指数相比并不优越;在一些研究中,ABSI 已被证明可以预测过早死亡率和心血管风险。然而,这两个指数都太复杂,对于日常使用来说也不方便。
因此,本研究提出了一种新的和简化的基于腰围的指数,腰围与BMI比率。在这个新指数中,WC代表内脏肥胖,BMI用于体型和质量的正常化。通过评估腰围与BMI的比率,并与传统的人体测量测量和较新的基于腰部的指数进行比较,以预测台湾T-SPARCLE登记处已确诊ASCVD患者的心血管结局。
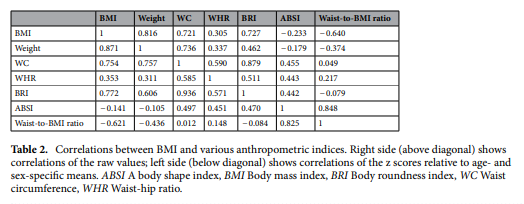
2010年1月-2014年11月共有6,920名ASCVD患者被纳入本分析,基线时平均年龄为65.9岁(SD 11.7),男性为73.9%,平均BMI为26.3(SD 3.8)kg/m2。其中,1.1%为体重不足,16.7%为正常体重,48.5%为超重,33.7%为肥胖。平均重量、WC和WHR分别为69.8(SD 12.4)kg、92.6(10.1)厘米和0.93(0.07)。在6,920例患者中,6,235例(90.1%)患有CAD,大多数为急性冠脉综合征(77.2%),4862例(70.3%)接受降脂治疗。其他基线临床和人口统计学特征列于表1中。随访时,58.2%、60.6%和67.5%的ASCVD患者分别达到最佳血清水平LDL-C<100 mg/dL、非HDL-C<130 mg/dL、TG <150 mg/dL(研究期间台湾健康保险指南的目标)。本研究队列中每个人体测量指数与BMI的相关系数如表2所示。

6,920名ASCVD患者被随访,中位时间为2.5年,227名患者经历了MACE。在ASCVD患者中,MACE的发病率为每100人年1.25(95%CI,1.10-1.42)。在针对分类 BMI 的多变量 Cox 回归分析中,ASCVD超重患者发生MACE的风险最低(调整后的 HR 0.61,95% CI 0.43–0.85,p = 0.004)(表3)。
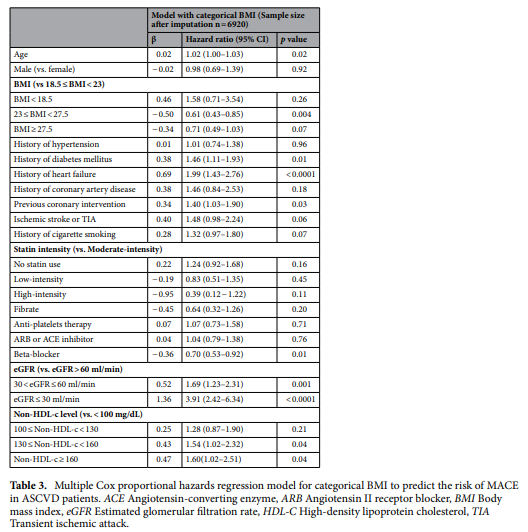
多变量Cox比例风险回归分析显示,在调整协变量后,腰围/ BMI比与MACE风险之间存在显著正相关(调整后的腰围/ bmi比增加的HR为1.69 / cm·m2/kg, 95% CI为1.12-2.49,p = 0.01)。 MACE的危险性随ABSI呈正相关增加,但差异无统计学意义(p = 0.06)。
然而,传统的人体测量参数,如BMI,体重,WC和WHR,或较新的腰围指数BRI,与MACE发病风险均无显著相关性(p = 0.09、0.30、0.89、0.54、0.79)(表4)。在限制性三次样条回归分析中,观察到传统人体测量参数或BRI与MACE风险之间存在u型关联(图1)。虽然ABSI或腰部与BMI比值与MACE风险之间的剂量 - 反应关联也是非线性的(非线性测试具有统计学意义,p 分别为= 0.049和<0.001),所有ABSI和腰- bmi比值范围内均存在正相关性。从限制性三次样条回归分析的图中估计拐点,发现腰围与BMI比值>3.6 cm·m2/kg时,MACE发生风险的增加更为陡峭(图1)。
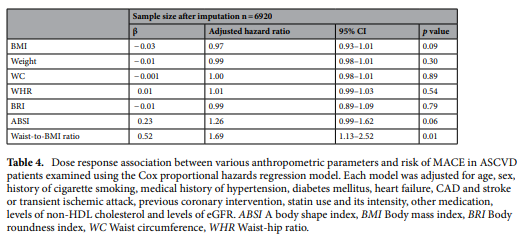
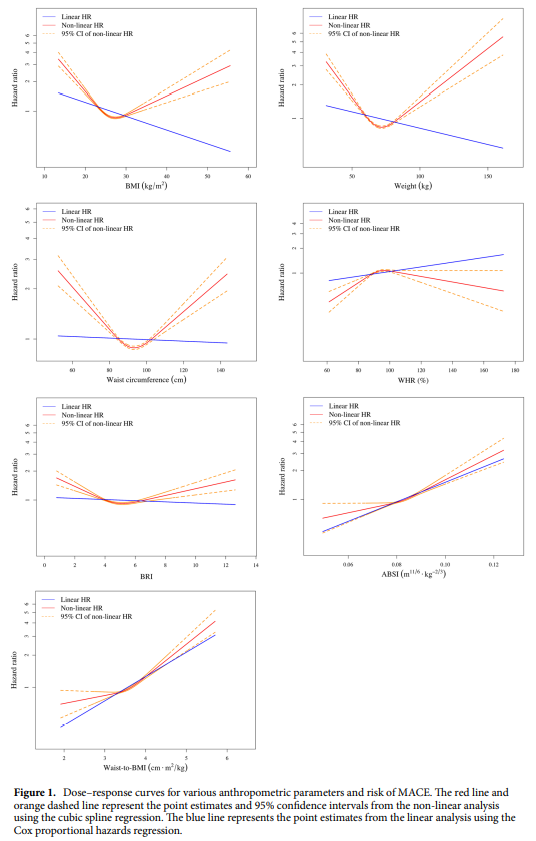
本研究再次观察到肥胖悖论,并且在分析分类BMI时,结果与以前的研究一致。随访期间超重的ASCVD患者发生MACE的风险最低。Cox比例风险模型和三次样条曲线回归分析均显示腰围与BMI比值与MACE风险之间存在正剂量-反应关联,尽管这种关联是非线性的。三次样条回归分析显示,ABSI与MACE风险的正相关形状与腰围-BMI比相似,但Cox比例风险模型的正关联不显著。BMI和其他传统的人体测量指标,如体重,WC和WHR,或较新的基于腰围的指数BRI,显示了与心血管结果的u型关联。
本研究结果表明,腰围与BMI比值是预测ASCVD患者心血管结局的良好阳性人体测量指标,特别是当该比值高于3.6 cm·m时2/kg,可以作为临床实践中一个简单、方便、有用的工具。
原文来源:
Chin-Feng Hsuan, et al. The waist-to-body mass index ratio as an anthropometric predictor for cardiovascular outcome in subjects with established atherosclerotic cardiovascular disease.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#疾病预后#
77
#粥样硬化性#
91
#粥样硬化#
76
#动脉粥样硬化性心血管疾病#
82
#硬化性#
86
#血管疾病#
71