Catheter Cardiovasc Interv:生物可吸收支架植入术可能作为分叉病变的治疗策略
2015-05-28 范伟译 MedSci原创
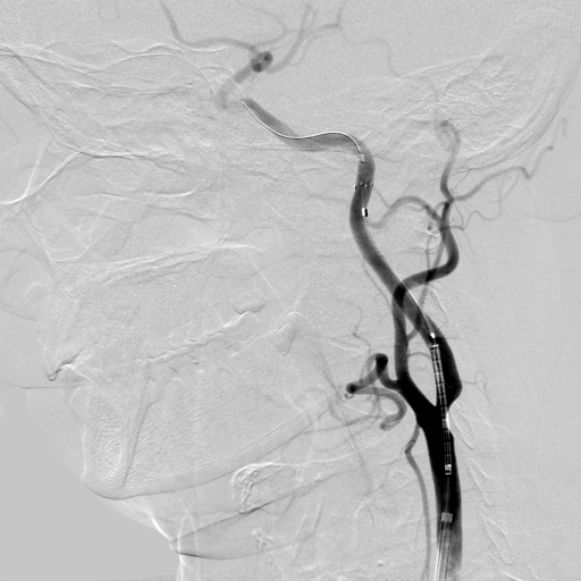
目的:本研究的目的是调研以生物可吸收支架(BRS)的临时支架(PS) vs双支架(DS)策略用于冠状动脉分叉病变治疗的临床结果。相关以生物可吸收支架植入治疗分叉病变的临床结果数据较为有限。方法:在2012年到2014年间,对132例生物可吸收支架BRS治疗分叉病变的病历进行了分析。在132例分叉病变中,10例病变没有用交叉支架治疗。99例病变(81%)用临时支架PS治疗策略,23例病变(
目的:本研究的目的是调研以生物可吸收支架(BRS)的临时支架(PS) vs双支架(DS)策略用于冠状动脉分叉病变治疗的临床结果。相关以生物可吸收支架植入治疗分叉病变的临床结果数据较为有限。
方法:在2012年到2014年间,对132例生物可吸收支架BRS治疗分叉病变的病历进行了分析。在132例分叉病变中,10例病变没有用交叉支架治疗。99例病变(81%)用临时支架PS治疗策略,23例病变(19%)用双支架DS治疗策略。双支架DS治疗组包含大量实质分叉病变的患者(PS 52.0% vs DS 91.3%:P < 0.001)。
结果:在PS组,7例病变(7.1%)通过T-支架搭桥。在DS组,13例病变(57%)以生物可吸收支架应用于分枝(SB)治疗。混合支架技术[生物可吸收支架应用于主枝治疗,和金属药物洗脱支架(DES)应用于分枝治疗]在10例(43%)病变中得以使用。在1年随访中,PS靶血管重塑(TLR)率为5.5%和DS靶血管重塑率为11.2%(P = 0.49)。任何分叉病变位点没有出现明显的支架血栓。
结论:这些发现表明,生物可吸收支架植入治疗分叉病变在技术上是可行的。在双支架DS策略组相比于临时支架PS策略组,靶血管重塑TLR率往往更高。亟待进行更大规模的研究,通过长期随访确定这种治疗策略。
原始出处:
Kawamoto H1,2,3, Latib A1,2, Ruparelia N1,2,4, Miyazaki T1,2, Sticchi A1,Naganuma T3, Sato K5, Figini F1,2, Chieffo A1, Carlino M1, Montorfano M1,Colombo A1,2. Clinical outcomes following bioresorbable scaffold implantation for bifurcation lesions: Overall outcomes and comparison between provisional and planned double stenting strategy.Catheter Cardiovasc Interv. 2015 May 27. doi: 10.1002/ccd.26045.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#可吸收#
55
#支架植入#
63
#ASC#
52
#生物可吸收#
56
看看
180
#植入#
51
#分叉病变#
59
#支架植入术#
58