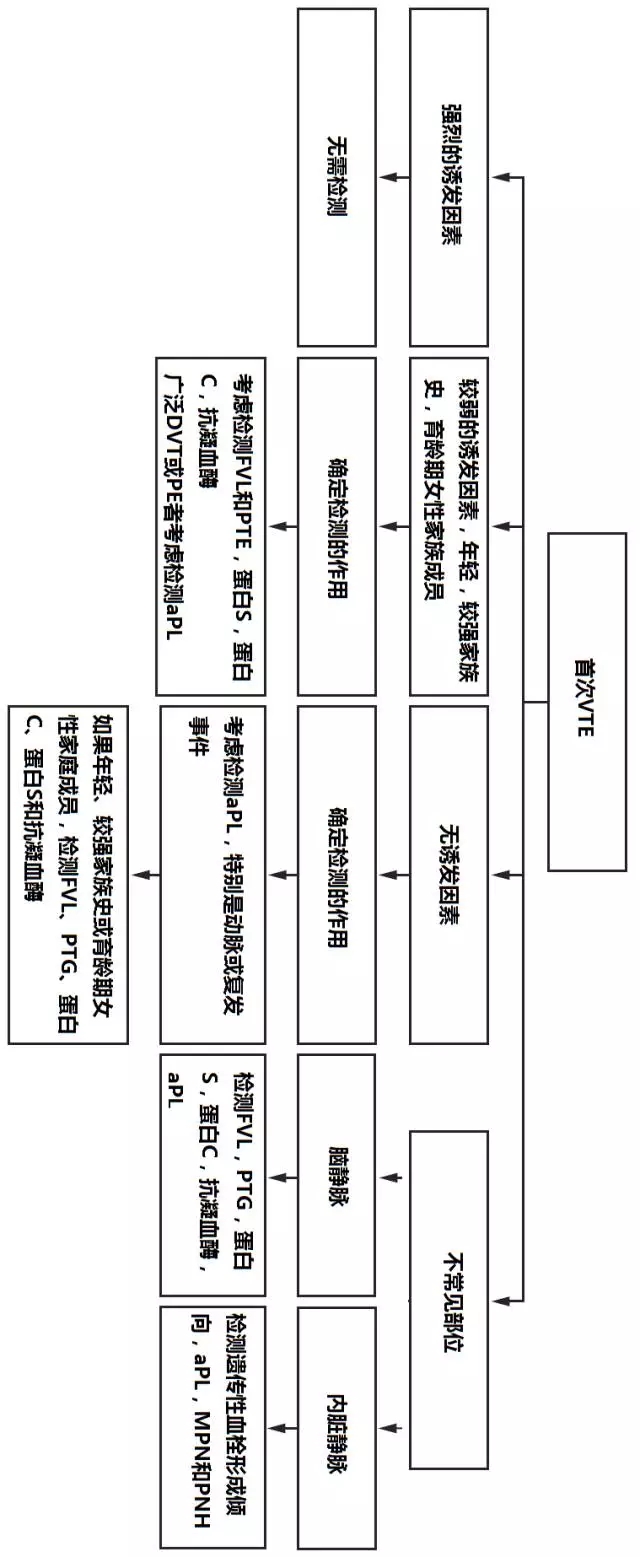
NEJM:血栓形成倾向检测流程和推荐意见
2017-10-05 杨中华 脑血管病及重症文献导读
在临床上经常进行血栓形成倾向检测;哪些患者需要检测,如何解读这些结果尚不清楚。截止到目前尚未发表血栓形成倾向检测的指南。ACCP-9指南以及2016年静脉血栓栓塞(VTE)更新版并未对血栓形成倾向检测给出指导性建议,2013年美国血液学会对于存在短暂性重要危险因素的VTE患者不推荐进行血栓形成倾向检测。英国血液病学委员会遗传性血栓形成倾向临床指南认为“关于何种患者或家属需要进行检测,不可能给出确切
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











非常好的文章.学习了
139
非常好的文章.学习了
153
好资料学习了!
153
学习
136
学习了谢谢分享!!
154
#血栓形成倾向#
122
非常好的文章.学习了
116
学习了新知识
123
谢谢分享.学习了
114