Circ-Cardiovasc Inte:经导管主动脉瓣置换术患者的临床结局及预后指标!
2018-03-16 xing.T MedSci原创
由此可见,TAVR是早期肝脏疾病患者重度主动脉瓣狭窄可行的治疗或是肝病根治前的过渡治疗。Child-Pugh B-C级患者、尤其是合并肾损害的患者,具有非常低的存活率,以及TAVR应慎重考虑以避免无效治疗。这些结果可能有助于改善肝病患者的临床决策过程和管理。
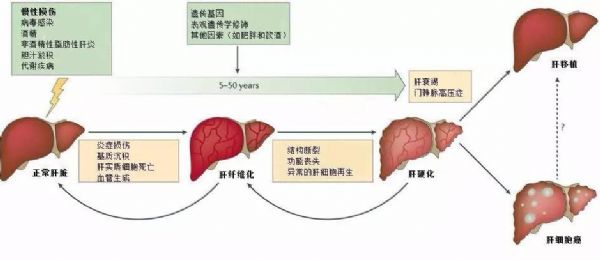
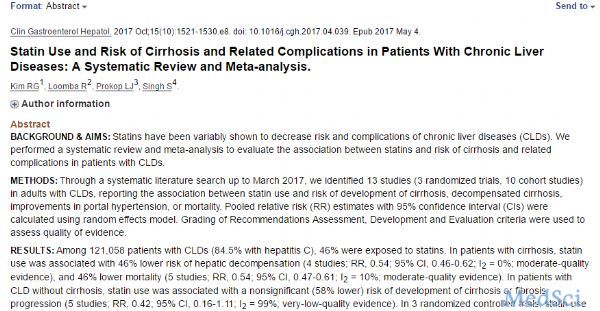
慢性肝病是心脏手术患者围手术期发病和死亡的已知危险因素。关于此类患者接受经导管主动脉瓣置换术治疗(TAVR)存在很少的数据。近日,心血管领域权威杂志Circulation: Cardiovascular Interventions上发表了一篇研究文章,研究人员的目的是评估接受TAVR治疗的肝病患者早期和晚期的临床结局,并确定这些患者死亡率的预测因素。
这项多中心研究收集的数据来自于114例慢性肝病患者,这些患者在12个机构接受了TAVR治疗。研究人员采用倾向评分的匹配分析(114对配对)比较了1118例无肝病患者的围手术期和远期结局。
研究人员发现匹配的组间住院死亡率、血管和出血并发症相似。急性肾损伤在肝病患者中较为常见(30.8% vs. 13.5%,P=0.010)。在2年的随访中,虽然组间心血管疾病的死亡率是相似的(9.4% vs. 6.5%;P=0.433),肝病患者非心源性死亡率也较高(26.4% vs. 14.8%;P=0.034)。较低的肾小球滤过率(估计的肾小球滤过率每减少5毫升/分钟的风险比为1.10;95%可信区间为1.03–1.17;P=0.005)和Child Pugh B或C级(风险比为3.11;95%可信区间为1.47–6.56;P=0.003)是慢性肝病患者死亡的预测因子,两个因素同时存在的患者(估计的肾小球滤过率<60 mL/min和Child Pugh B或C级)2年随访的死亡率为83.2%。
由此可见,TAVR是早期肝脏疾病患者重度主动脉瓣狭窄可行的治疗或是肝病根治前的过渡治疗。Child-Pugh B-C级患者、尤其是合并肾损害的患者,具有非常低的存活率,以及TAVR应慎重考虑以避免无效治疗。这些结果可能有助于改善肝病患者的临床决策过程和管理。
原始出处:
Gabriela Tirado-Conte,et al. Clinical Outcomes and Prognosis Markers of Patients With Liver Disease Undergoing Transcatheter Aortic Valve Replacement A Propensity Score–Matched Analysis.Circulation: Cardiovascular Interventions.2018. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005727
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
60
#经导管主动脉瓣置换术患者#
68
#临床结局#
60
#置换#
59
#主动脉瓣置换术#
64
#置换术#
57
#经导管主动脉瓣置换#
65
#经导管#
77
#主动脉#
65
#预后指标#
75