Gastroenterology:炎症性肠病的妇女接受生物制剂和硫唑嘌呤治疗对于新生儿结局的影响
2021-03-18 MedSci原创 MedSci原创
有研究显示患有炎症性肠病(IBD)的孕妇更容易发生自然流产(SAB),早产,以及分娩和分娩期间的并发症的出现。因此,需要用药物治疗保持怀孕期间的病情稳定。
有研究显示患有炎症性肠病(IBD)的孕妇更容易发生自然流产(SAB),早产,以及分娩和分娩期间的并发症的出现。因此,需要用药物治疗保持怀孕期间的病情稳定。目前来说治疗IBD的主要方法有硫嘌呤(硫唑嘌呤,6-巯基嘌呤);生物制剂(抗肿瘤坏死因子(TNF)拮抗剂(英夫利昔单抗,阿达木单抗),抗整合素(vedolizumab,维丽珠单抗珠单抗),抗白介素12/23(ustekinumab);或生物和硫嘌呤的组合等等治疗方案。但是动物暴露于超治疗剂量的硫嘌呤会产生先天性畸形,但是人体研究并未显示出明显的风险。因此,本项研究就旨在探究怀孕期间的IBD治疗对母亲和孩子的健康产生了哪些影响。

在2007年至2019年之间,研究人员对美国的IBD孕妇进行了一项前瞻性,观察性,多中心研究。初步分析是比较子宫内未接触生物制剂,硫代嘌呤或二者结合的5种妊娠结果(先天性畸形,自然流产,早产,低出生体重和婴儿感染)的发生率。使用双变量分析,然后对相关混杂因素进行调整的逻辑回归模型用于确定特定药物类别对目标结果的独立影响。
在完成的1490例孕产妇中,有1431例活产。暴露于硫嘌呤的有242名患者,暴露于生物制剂的有642名患者或两者联合治疗的有227名,未暴露的患者有379名。在出生后的第一年,接触药物并不会增加先天畸形,自然流产,早产,低出生体重和感染的发生率。较高的疾病活动性与自然流产的风险(OR,3.41; 95%CI,1.51-7.69)和早产与婴儿感染增加相关(OR,1.73; 95%CI,1.19-2.51)。
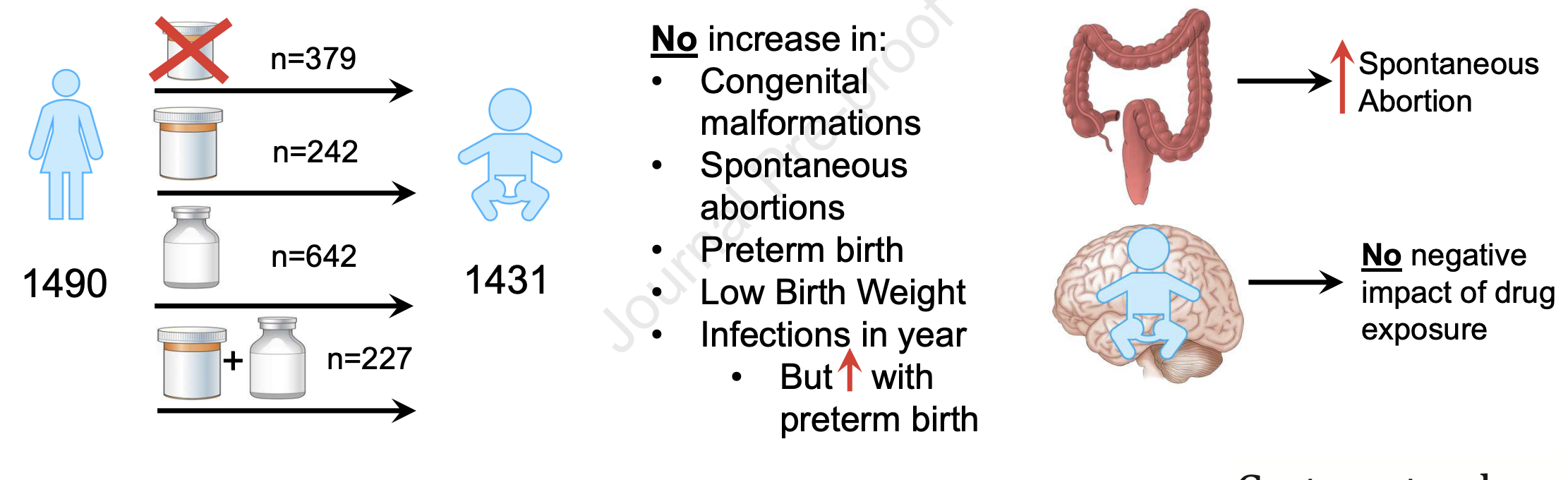
怀孕期间的生物制剂,硫嘌呤或联合治疗暴露与出生时或生命的第一年母体或胎儿不良预后增加无关。对于患有IBD的女性,可以在整个妊娠期间继续使用这些药物进行治疗,以保持疾病控制和减少与妊娠相关的不良事件的发生。
原始出处:
Uma Mahadevan. Et al. Pregnancy and Neonatal Outcomes After Fetal Exposure to Biologics and Thiopurines Among Women With Inflammatory Bowel Disease. Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#生物制剂#
146
#AST#
84
#GAS#
82
#Gastroenterol#
69
#Gastroenterology#
114
#炎症性#
58
学习了
95