Nature Methods:科学家研发人工胸腺,有望逆转癌症治疗
2017-04-05 佚名 来宝网
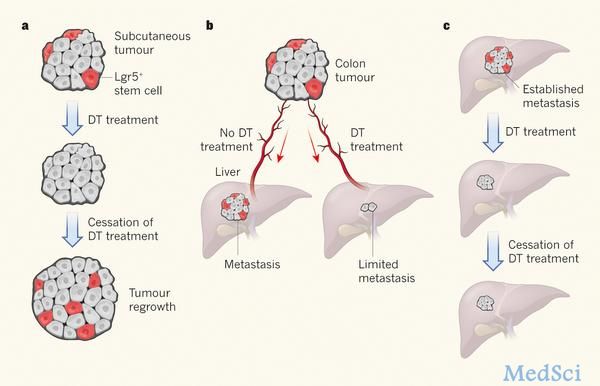
加州大学洛杉矶分校(UCLA)的研究小组创建了一个全新的系统来产生人类T细胞,这种白细胞可以对抗外来病毒的侵略,系统工程师可以利用这一系统来发现并攻击癌细胞,这就意味着我们向战胜癌症又前进了一步。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胸腺#
78
#癌症治疗#
69
#研发人#
120
#MET#
86
#Nat#
82
#研发#
115
反复实践,反复学习,认真推敲,不断提高自己的业务水平。
92