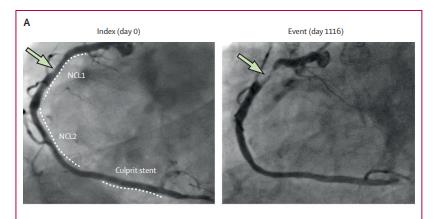
Lancet:近红外光谱-血管内超声联合应用评估非梗阻性病变的未来风险
2021-03-13 MedSci原创 MedSci原创
对于冠状动脉病变患者,其非梗阻性病变经近红外光谱和血管内超声联合评估,可对患者未来不良心脏结局的风险做出更为准确的预测

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
94
#近红外#
95
#红外光谱#
98
#联合应用#
91
#非梗阻性#
0
顶刊就是不一样,质量很高,内容精彩!学到很多
109
好文章!
161