Surg Neurol Int. :具有先天性皮肤血管瘤的脊椎背侧 D1-D7 血管瘤的硬膜外延伸的病例报告
2021-10-09 MedSci原创 MedSci原创
多发性椎体血管瘤 (MVH) 通常累及多个椎体,偶尔会延伸到硬膜外腔。它们占所有脊柱肿瘤的 2-3%,并且通常遵循惰性、无症状的过程。然而,由于硬膜外脊髓压迫、病理性骨折和/或出血的组合,一部分可能会
多发性椎体血管瘤 (MVH) 通常累及多个椎体,偶尔会延伸到硬膜外腔。它们占所有脊柱肿瘤的 2-3%,并且通常遵循惰性、无症状的过程。然而,由于硬膜外脊髓压迫、病理性骨折和/或出血的组合,一部分可能会出现明显的脊髓压迫症状/体征,需要手术。在组织学上,MVH 分为以下三类之一:毛细血管、海绵状、动静脉或静脉型。
案例描述:
一名 24 岁男性因多发性脊椎血管瘤 (MVH) 伴硬膜外延伸(即导致 D1-D3 显着脊髓压迫)而出现6个月的进行性下肢轻瘫,以及 D2-D7 水平的先天性皮肤病变。术前血管栓塞后,进行了 D1-D7 椎板切除术以及 C7-D8 椎弓根螺钉固定。病理上,骨和皮肤病变为脊髓海绵状血管瘤。术后,患者恢复正常功能。由于无法完全切除,他随后接受了放射治疗以防止肿瘤复发。

患有先天性胸部、手臂和前臂皮肤血管瘤的患者(左)(a)前部和(b)后部。
神经病学
检查时,他的下肢弥漫性运动强度为 3-4/5,相对感觉水平低于 D4 水平,没有括约肌受累。
CT结果
胸CT显示不规则溶骨性病变粗加厚小梁涉及到D7的D1椎骨水平,还包括左1到6肋。轴向研究显示椎体受累的典型“圆点”模式。在受累椎骨附近还有左侧椎旁和小管内增强软组织增厚,导致明显的脊髓受压。
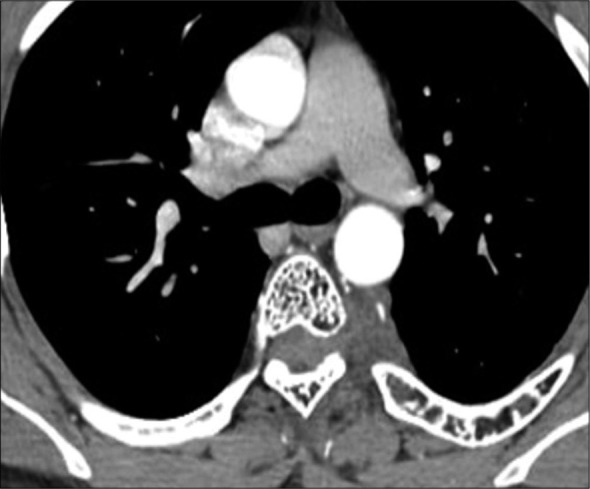
胸椎 CT 轴位图显示“圆点”外观。
磁共振检查结果
在 MR 上,肿瘤在 T1W 和 T2W 图像上都是低信号的,并通过对比增强(即,通过椎间孔扩展包裹了从 C7 到 D8 的颈背脊髓)。在 D2-D3 椎体水平也观察到脊髓内 T2W 高信号的微妙增加。
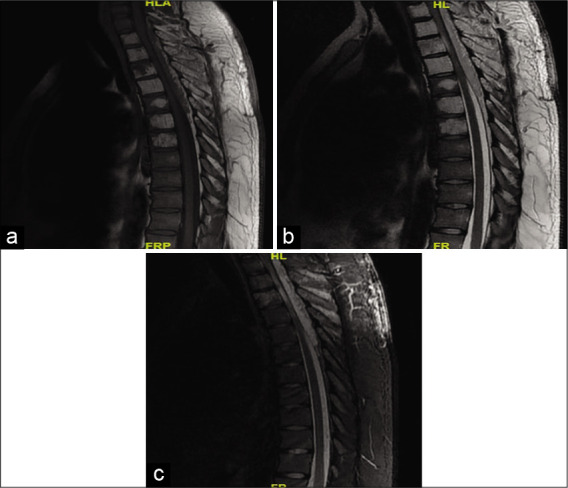
MRI 背脊矢状面 (a) T1W 图像 (b) T2W 图像 (c) STIR 图像显示涉及 D1-D7 椎骨的骨髓信号强度改变,在 T1W 和 T2W 图像上均出现低信号,后部元件连续受累。在 D1-D7 椎骨中观察到片状残留正常骨髓信号。由 C7 至 D8 椎骨引起的硬膜外/硬膜外病变在 T1W 上呈低信号,在 T2W/STIR 上呈高信号,对颈背脊髓造成显着的占位效应。D2-D3 水平的 Intracord T2W/STIR 高信号。
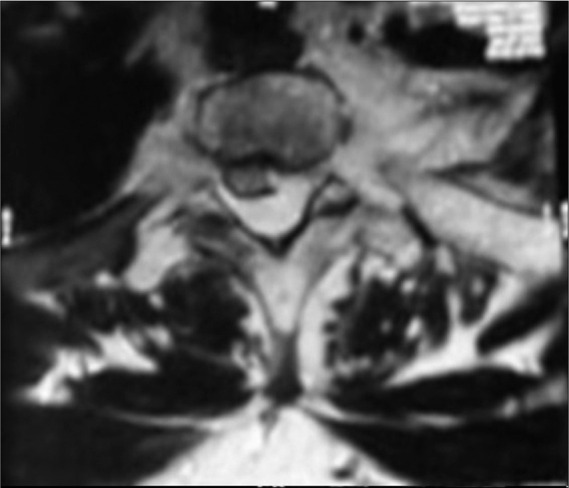
MRI 背脊轴位 T2W 图像显示左肋椎关节和相邻肋骨的连续浸润,骨髓信号明显改变。浸润性硬膜外/硬膜外病变对脊髓造成显着的占位效应,并显示脊髓向右侧移动。
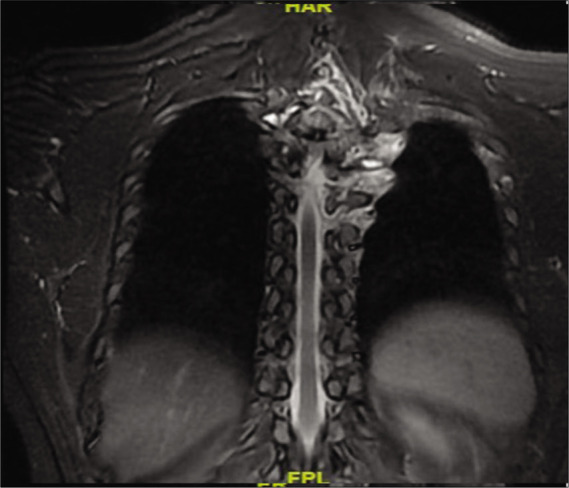
MRI 背脊冠状位/STIR 图像显示左侧多个水平的肋椎关节连续受累。
外科手术
在 D1-D7 椎板切除术后,发现一个红褐色、柔软的病变,并伴有血管。肿瘤附着于背侧鞘囊,并表现出外侧、椎间孔和左侧椎旁延伸。图 6a]。血管被凝固并被切除[图 6b]。最后,患者接受了从 C7 到 D5-D8 的椎弓根螺钉融合术。
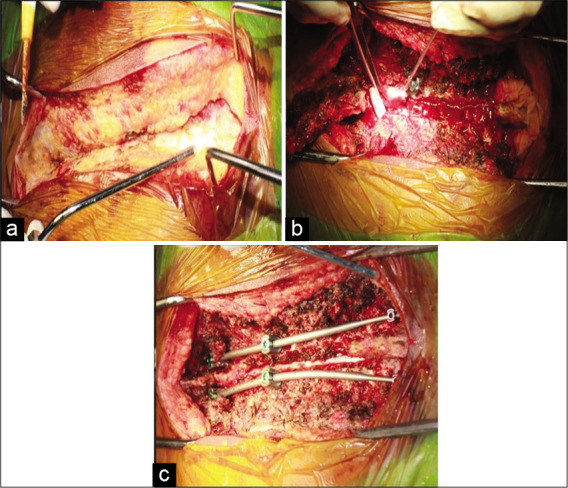
术中图片 (a) 背椎上方脊髓旁软组织中的血管瘤病变 (b) 椎板切除术后暴露硬膜外病变包裹脊髓后部 (c) 使用椎弓根螺钉和连接杆对脊髓和器械进行减压。
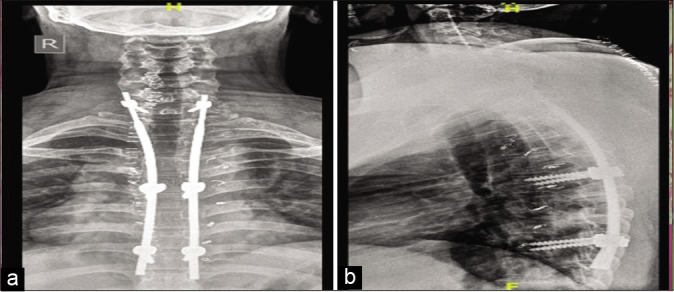
术后 X 射线背脊 (a) AP,(b) 侧视图。
病理
冰冻切片(即硬膜外、椎板、椎旁和皮肤)均与海绵状血管瘤一致。
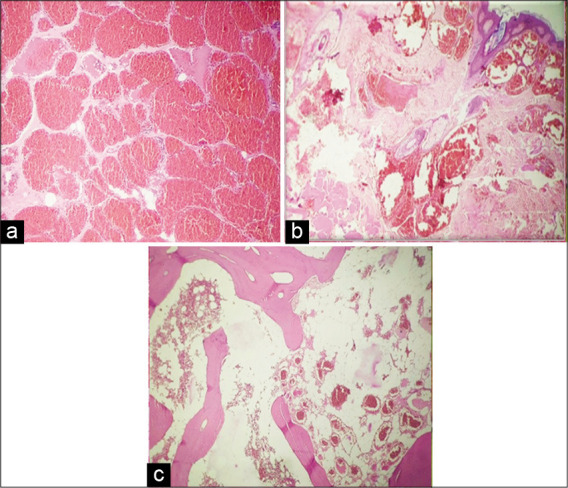
组织病理学检查显示海绵状血管瘤(a)扩张和充血的不同大小的血管间隙(b)真皮显示扩张和充血的血管(箭头)。
真皮显示出血 (c) 骨,骨髓显示充满血液的紧密填充的扩张血管空间。
术后恢复
患者恢复顺利;1 周后,出院时,他的情况有所好转,能够毫无虚弱地走动。两个月后,他的双侧肌肉力量为 5/5。
术后辅助放射治疗
患者术后对瘤床进行放疗,以治疗手术难以触及的肿瘤,并限制复发的机会。
讨论
根据世界卫生组织的分类,椎体血管瘤被认为是一种良性的骨血管形成性肿瘤。最常见的部位是胸椎(约 60%),其次是颈椎(30%)和腰椎(10%) .这些病变通常局限于椎体,但偶尔可能会扩展到椎弓根、弓和棘突。值得注意的是,绝大多数椎体血管瘤是无症状的,通常在放射影像学检查或 仅在 1% 至 2% 的病例中可以看到椎体血管瘤的进一步硬膜外延伸,导致缓慢进展的压迫性脊髓病或神经根病。
在我们介绍的案例中,患者患有与椎骨/硬膜外肿瘤部位相同水平的先天性皮肤血管瘤。然而,一些文献描述了与脊髓血管瘤相关的肝、脾等其他器官同时发生血管瘤的病例。
磁共振成像是脊髓血管瘤最可靠的检查。建议术前行脊柱血管造影术,术前应做供血血管栓塞术,避免术中大出血风险。椎板切除术是一种有效的减压手术,不会导致不稳定或畸形。但是,如果发生椎体压缩性骨折,则可能需要进行椎体成形术和/或融合术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#硬膜外#
91
#Neurol#
95
#血管瘤#
106
#先天性#
109
#病例报告#
156
#脊椎#
88
学
107
内容实用,已下载
125