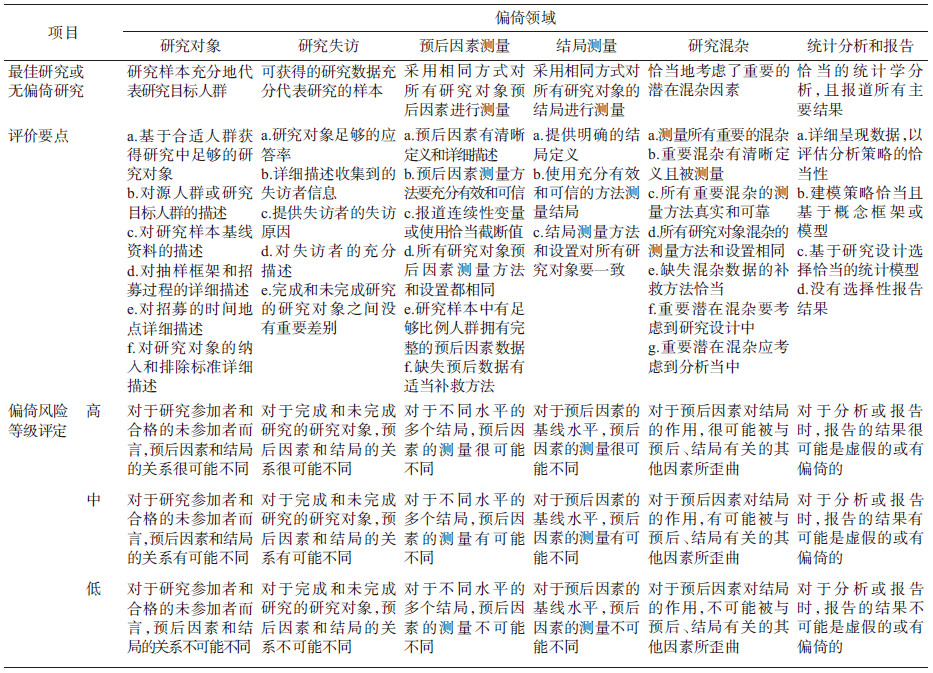
采用QUIPS(Quality In Prognosis Studies)工具对预后因素研究中出现的偏倚进行评估
2019-09-25 唐少文, 张渊, 陶必林, 杨智荣, 孙凤, 詹思 中华流行病学杂志
疾病预后研究(prognosis studies)是指对疾病发展为不同结局可能性的预测与影响因素研究。预后研究有助于医患双方了解疾病的发展趋势,并做出相应的临床决策,以争取较小的代价与较好的疾病转归[1]。预后因素(prognostic factors)是预后研究的重要内容之一,主要是指能预测疾病某种(些)结局发生时间与概率,或者能改变结局发生进程与概率的因素[1]。预后因素研究可以借助于各种
疾病预后研究(prognosis studies)是指对疾病发展为不同结局可能性的预测与影响因素研究。预后研究有助于医患双方了解疾病的发展趋势,并做出相应的临床决策,以争取较小的代价与较好的疾病转归[1]。预后因素(prognostic factors)是预后研究的重要内容之一,主要是指能预测疾病某种(些)结局发生时间与概率,或者能改变结局发生进程与概率的因素[1]。预后因素研究可以借助于各种流行病学方法,但研究过程中存在各种偏倚会导致研究结果无法在人群中进行预测或验证[2]。因此,有必要对预后因素研究中存在的偏倚风险进行评估,以便筛选出合格研究后再进行证据整合,从而为临床循证决策提供基础。 一、制定背景 在开展预后研究系统综述时,纳入的原始研究如果在方法学上存在缺陷将会直接影响系统综述的内部有效性,导致无效的结果或推论。然而,对如何评估预后研究的质量尚无一致的共识。Hayden等[2]2006年通过检索Medline上1966-2005年11月之间发表的预后研究系统综述,纳入基于队列研究且有质量评价的系统综述共163篇,然后提取每篇系统综述内进行质量评价的条目(共计882项)。两位资
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#QUIPS#
48
#studies#
56
#prognosis#
62
#iPS#
57
#预后因素#
57
#DIE#
54
#PRO#
46